Stem Cells and Prolotherapy
Stem cells and prolotherapy? Prolotherapy is an injection technique whereby certain solutions are injected to cause an inflammatory healing response. We’ve used the technique for years to tighten lax ligaments and get rid of tendon related pain. We’ve published research on prolotherapy and based on our experience, this is a great technique that if applied by every family doctor could save the US health care system billions of dollars.
Having said that, recently we became aware of physicians offering cellular therapy (PRP and/or stem cells) with prolotherapy, which regrettably means that these physicians are injecting dead cells. Let me explain. Prolotherapy works in part by causing local cellular injury to an area, similar to debridement of a non-healing wound. For example, it’s been known for centuries that “roughing up” (debriding) a non-healing wound will result in that wound slowly progressing toward being healed. The same applies to prolotherapy, where the solution injures or kills the superficial layer of cells in order to chemically “rough up” a non-healing area, which causes healing resources to hone in on the spot. In essence prolotherapy works by giving you another bite at the healing apple. However, add stem cell or platelets to that mix or inject one and then the other in the same space and the injected cells will quickly perish. Why?
Prolo works by osmotic action, it’s a hyper-concentrated solution that sucks the water out of the cells it touches. If those cells are layered deep, then only the superficial cells would be impacted, causing a pro-inflammatory healing response, just like a cosmetic laser kills off the superficial layer of skin cells to rejuvenate the skin. However, if those cells are in solution (like stem cells and platelets), they will quickly shrivel and die while the water is sucked out of the cell. If the physician is using prolotherapy and PRP (platelet rich plasma) together, the good news is that while the platelets will be “lysed” (imploded), large amounts of helpful growth factors in the platelets will be released into solution. There would be clinical situations where this would be an advantage and other times when it would be a disadvantage, but you still end up with a solution that’s likely a net positive to the patient.
However, add prolotherapy solution to stem cells and you get a different story. While platlelets are important because they contain growth factors and these help healing, stem cells are important for their growth factors (which they manufacture), for coordinating a local repair response (like a general contractor), and for differentiating into a cell type that needs replacement or repair. So if you implode a stem cell, you might get a few growth factors, but the other two functions are lost.
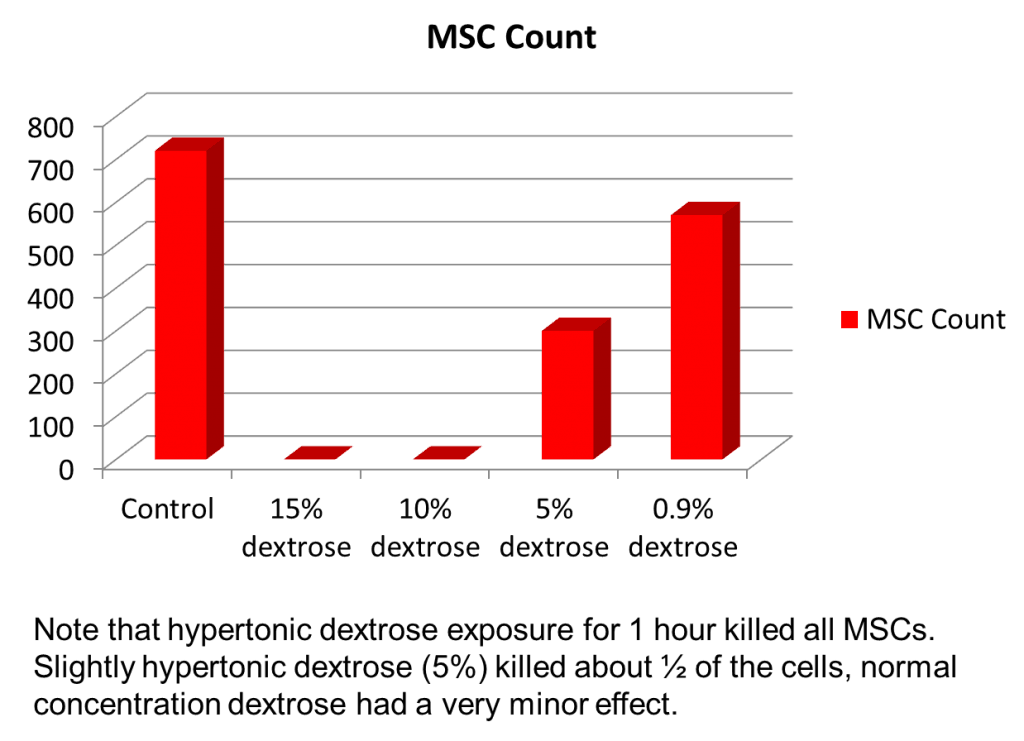
How do we know this? We have an advanced lab where we performed this experiment in 2007 and ended up with dead stem cells. Note the data above from an experiment where mesenchymal stem cells from bone marrow were exposed to various concentrations of prolotherapy solution. Most prolotherapists use 10-15% dextrose. In both the 10% and 15% dextrose cases, the stem cells were killed dead (note that the height of the bar is the surviving stem cell count with the control bar being how many stem cells should be there). Even at a very low concentrations of dextrose (5% is very low from a prolotherapy perspective), most of the cells were killed. Therefore using stem cells and prolotherapy in the same space means you get dead stem cells that won’t help the patient much.
The upshot? Using prolotherapy and PRP likely has it’s benefits, but using prolotherapy and stem cells together is a recipe for lots of ineffective, dead stem cells. Does this mean the two can’t be used together? No, we use prolo in patients to tighten ligaments keeping the prolotherapy and stem cell treatments far apart in time so that the hyper-concentrated solution is diluted by the body and won’t impact the stem cells.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.