Suffering from a Meniscus Tear? Why Arthroscopic Knee Surgery Isn’t the Answer
For several decades in orthopedic care, the traditional solution to meniscus tears has been to identify them on an MRI and cut out the offending piece. While there’s little doubt that meniscus degeneration is at play in the cascade of knee arthritis, how all of this works is not so well understood. Now, a new study continues to point in the direction that meniscus surgery is likely the exact opposite of what we should be doing to help middle-aged patients with knee pain.
What is the Meniscus?
Hank Grebe/Shutterstock
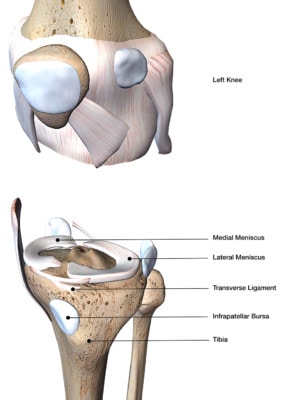
The meniscus is a spacer that helps to cushion the knee cartilage. This structure can get normal tears as we age, much like your face naturally wrinkles over time. While a huge industry has emerged around removing parts of the meniscus when tears are seen on an MRI, there’s little hard scientific evidence that this is a good idea.
Alternatives to Arthroscopic Knee Surgery for a Meniscus Tear
To understand why the science now supports that our whole surgical approach to treating meniscus tears is ill-advised, let’s follow a 45- year-old patient who develops knee pain when hiking or running. The patient moves suddenly to avoid a rock, hears a pop in his knee, and his knee begins to swell. All of a sudden, an otherwise active middle-aged guy can’t hike or run without pain. At first the patient tries to ignore it, but after a week of no improvement, he visits the family doctor. An MRI shows some swelling and a meniscus tear and our guy is referred to an orthopedic surgeon.
Let’s stop our story right here for a moment. While the patient and his physicians are convinced they have found the source of his knee pain, the hardcore research of the last few years tells a different story. In fact, it’s highly likely that, had we performed the MRI months before the knee was injured, we would’ve seen the same tear! Additionally, if we performed an MRI on our patient’s 10 best buddies, all of whom have no knee pain, about half would show a meniscus tear that looked just like our patient’s. So regrettably, the meniscus tear is a “red herring”, not a diagnosis.
Surgical Meniscus “Repair” is Usually Code for Meniscus Removal
Let’s stop our story again here and recall that the surgery to “repair” the meniscus has been shown in multiple studies to be no better than a fake or placebo surgery . Hence, we have no scientific evidence that this procedure will help this patient’s knee. In fact, other studies show that in all likelihood, removing some of the knee meniscus will only cause more knee arthritis.
While the likeliness of knee arthritis after a meniscus surgery seems to be due to less cushioning in the joint for protecting the cartilage, another reason may be that removing the damaged cells is the last thing the degenerating meniscus needs.
Your Meniscus is Alive!
It’s easy to conceptualize the knee meniscus as just an inanimate object, like a gasket or rubber piece in the mechanical engine that is your knee. However, it’s actually living tissue that’s made up of cells. A recent study makes a fine point of this by using sophisticated immunostaining to observe the number of living cells in the meniscus. The researchers found that there were fewer functional cells in the degenerated meniscus tissue that show tears on an MRI. This finding is important for the patient mentioned in the sequence of events described above and anyone else suffering from knee pain due to meniscus tears.
For example, if degenerating meniscus tissue leads to tears—which usually have nothing to do with why the knee began hurting—then removing the torn piece decreases the total number of meniscus cells left in the knee, logically leading to the progression of arthritis. So shouldn’t we be adding cells instead of removing them?
Let’s take the wrinkle analogy discussed above. If meniscus tears are about as clinically meaningful as face wrinkles, what if our solution to the latter problem was to surgically remove each wrinkle? It wouldn’t be long before the face was a mess! In this analogy we can clearly see that it would be far better to inject something to plump up the skin and get rid of the wrinkle for a time, which is what’s done with collagen shots in cosmetic clinics. This is also done in orthopedic clinics when hyaluronic acid gel shots are injected for knee arthritis. In addition, like our meniscus tissue, the research shows that the wrinkles are caused by a decrease in the number of living cells, which leads to fewer extra-cellular matrices being produced. Hence, injecting cells into the wrinkle would also do the trick!
The upshot? Removing parts of a meniscus is not a smart idea, despite the fact that a multi-billion dollar medical industry has thrived on the outdated concept. This is not only because the meniscus is an important cushion protecting the knee, but also because we should be adding cells to the knee, not removing them! So how can we add cells to a knee meniscus? We do this every day around the Regenexx Network with one of our patented Regenexx procedures, which uses precise ultrasound guidance to inject the knee meniscus with the patient’s own stem cells. Because we believe in facing the problem head on instead of ignoring the consequences that will pop up later on down the road.
Challenge the old doctrine of cell removal as a solution and consider reinvigorating your knee with stem cells instead. Your decision could mean the difference between a temporary fix and chronic pain—or healthy knees that will last you a lifetime.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.