Bone Spur Pain – Why Relief May Be Simpler Than You Think
A patient who recently read my post about why you should avoid surgical hip bone spur removal, asked a question about the x-ray above. She has a number of symptoms and her doctors have told her that this picture explains why she hurts. Does this image really show that, or are these bone spurs a symptom of something else?
When you’re hurting and nobody seems to be able to help, it’s frustrating. So when a picture shows something, however small, it’s only natural that a patient looking for answers will grasp that finding with both hands. However, what’s often being conceptualized as a cause, is really just another symptom. And in this case, it’s one that you can see on an x-ray.
This article addresses this patient’s concern about pain as it relates to her hip bone spurs, but keep in mind that the general concept applies to most all areas where bone spurs are found. A bone spur is typically a symptom of some other musculoskeletal problem and may not be causing the actual pain. More often than not, surgically removing bone spurs is not the best option.
Understanding Bone Spurs
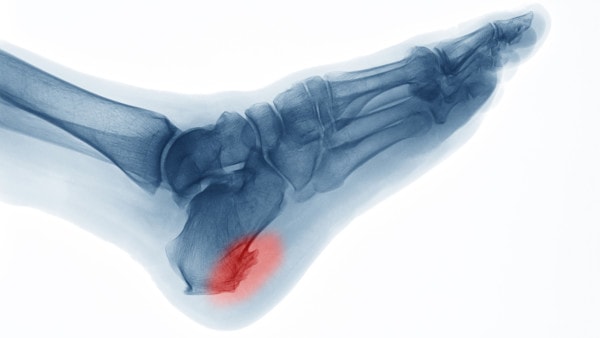
Suttha Burawonk/Shutterstock
To understand how to interpret the image above, you have to understand a little about bone spurs and what causes them. A bone spur can form when there’s too much pulling on bone. For the most part this is not a problem, but a symptom of instability. When a joint is moving too much or is moving in the wrong direction, the covering of the joint (capsule) where it attaches to the bone can get yanked on more than it should. The same can happen with muscles that attach around the joint. The body creates the bone spur to shore up the capsule or tendon attachment, in essence trying to make it stronger. The good news is that this works in some ways. The bad news is that the normal shock absorbing properties of the tissue is reduced.
Is this patient’s pain actually coming from bone spurs?
This patient describes her problems as:
“The pain is in my buttock (perhaps my gluteus maximus), runs down the IT band and the muscle in the back of my leg (behind my femur) from my buttock to my knee. The pain is debilitating at times, to the point that I take a tramadol just so I can go about a daily routine…I have been through a month of physical therapy (no relief) and this week saw a rehab specialist that is in with a chiropractor that my daughter sees. He showed me how to stretch out the IT band and used the tens unit on my hip and thigh.”
So what causes pain in the buttocks that radiates down the outside of the hip and thigh, or iliotibial band? The most common issue we see is an irritated nerve in the low back. This can happen in patients with and without low back pain, as this symptom is usually their early warning sign of a nerve issue in the low back.
It’s usually hard for patients to understand that they can have a low back problem without pain in their low back. This is because they have been taught that the first sign of a low back issue is low back pain. However, if I were to reach in and irritate your L5 nerve in your back, you wouldn’t feel back pain, but only radiating pain or other symptoms in your butt and down your IT band!
Why did these bone spurs form?
How do bone spurs have anything to do with irritated nerves in the low back? Nerves drive muscles. In fact, without a healthy nerve the muscle begins to get weaker, and if the nerve is sick enough, it will eventually die off. In this case, an irritated nerve in the back leads to weakness in the hip girdle muscles. This then leads to a hip joint that can’t control its motions well. The muscles and hip capsule then get yanked on, which causes the bone where they attach to protect itself by growing a bit bigger. In this case, the L5 nerve problem caused the muscles to get weak and the bone spurs to form. She feels it as pain and tightness down the outside of her hip.
How is this issue treated?
As an example, think about a car’s front end alignment. The front tires will wear unevenly. Parts of one or both tires will become bald. Now let’s say your mechanic proposed that the wear on your tires was the real problem and ignored the alignment. That he needed to perform a “surgery” of sorts to cut out the parts that weren’t worn and make your tires better. This of course would never fix the real problem, so your tires would just wear down until they popped!
The upshot? The good news is that at this point nobody is offering to remove these hip bone spurs, but given the propensity of the orthopedic surgical community to want to remove these “symptoms”, that may well be offered to her at some point. In the meantime, this patient needs to ensure her providers are focused on what’s causing the spurs in the first place!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.