Epidural Steroid Injection Risks: New FDA Epidural Steroid Warning?
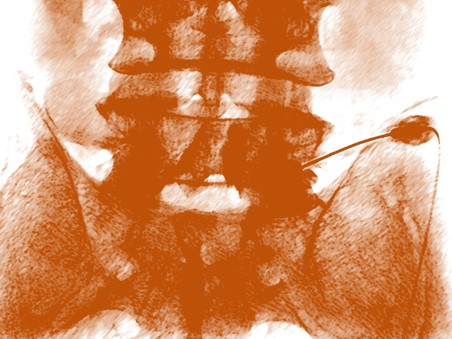
Epidural steroid injection risks are in the news again. First, I am not a big fan of epidural steroid injections. These injections are imaging guided procedures where a steroid (potent anti-inflammatory) is placed between a bulging or herniated disc and a painful nerve that’s causing sciatica. The good news is that they’ve dramatically reduced low back surgery rates in the US in the last 15 years, the bad news is that spine surgeons have found another way to keep operating-low back fusion. However, I cringe a bit every time I’m forced to do one of these injections, as the steroid dose used by almost all physicians performing the procedure is way too high. As an example, if the normal amount of steroids your body manufactures were represented by the height of a matchbook, the amount being injected in the average epidural steroid injection is the height of the Empire State Building! Now the FDA is warning that it never approved these steroid medications for this use-which is both a good thing and an unnecessary thing when one reads the warning.
Steroids are powerful anti-inflammatory drugs. They also have their dark side when delivered in high doses (which is the standard milligram range). They can lead to local cell death and in the case of epidural steroid injections, an increase in fracture risk in women that’s likely due to the steroids hurting bone metabolism. On the other side of that coin, epidural injections, properly performed under fluoroscopic guidance by highly skilled physicians, save hundreds of thousands of patients a year from unnecessary and potentially harmful spine surgery. What’s fascinating is that some ground breaking and head turning research by Manchikanti et. al. has shown that the injections work just as well with or without the steroid (cervical, lumbar)! Meaning that it’s likely the anesthetic that’s providing the relief and not the potentially harmful steroid. Our results with anesthetic only epidural injections haven’t been as good, so we instead have just reduced the dose to closer to the body’s physiologic amounts (the matchbook height) and added natural growth factors from the patient’s own blood platelets to prompt healing.
The FDA got dragged into epidural steroid injections due to the compounding pharmacy tragedy where contaminated vials of steroid were used which resulted in life threatening infections. Let’s look at their warning from the FDA web-site:
ISSUE: FDA is warning that injection of corticosteroids into the epidural space of the spine may result in rare but serious adverse events, including loss of vision, stroke, paralysis, and death. The injections are given to treat neck and back pain, and radiating pain in the arms and legs. The effectiveness and safety of epidural administration of corticosteroids have not been established, and FDA has not approved corticosteroids for this use.
To the untrained eye, this warning, which was copy and pasted into numerous medical news stories, seems reasonable. No doctor or patient ever wants a single serious adverse event. However, the problems listed have long since been addressed by the interventional pain management community going back to the mid-1990s. Back then, as many new physicians began to use these procedures, a disturbing and rare side effect profile was noted due to the use of particulate steroids (steroid preparations which had big particles floating in them). These particles, if inadvertently injected into a small artery, would block the flow of blood to part of the spinal cord and cause paralysis. The interventional pain management community responded and almost all competent and well trained physicians no longer use this type of steroid.
What about the other side effects like stroke or loss of vision? These again are easily preventable by technique. The only way this could really happen is in a cervical epidural where the doctor injects into the vertebral artery. The steroid however is very unlikely to cause these issues; it would be the anesthetic that would cause big problems. The other side effects noted are all related to technique again. They are usually caused by inadvertent injection of the anesthetic (not the steroid) into the dura (covering of the spinal cord and nerve roots) and are either short lived problems lasting hours or can be easily managed by experienced personnel.
In the FDAs defense, they also said they were convening a panel of experts to try to come up with solutions to solve these “problems”. However, those solutions have been known and widely disseminated for more than a decade. In addition, the fact that FDA is involving itself in how the steroids are used (which is the practice of medicine) is a slippery slope, as much medical innovation occurs through non-FDA regulated “off-label” use where a physician finds new uses for medications. So FDA asserting authority into how off label use occurs is very concerning to doctors and patients.
The upshot? There is no longer any reason to use high dose steroids in epidural injections, save for a few patients where this could make the difference. This is because these powerful anti-inflammatory drugs have big side effects. Having said that, the FDA is now trying to solve a problem that was solved a decade ago. There will always be bad doctors with poor training who do these injections wrong and hurt patients, however, that why state medical boards exist. So while well meaning, the FDA’s involvement in off-label use is very concerning.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.