Why Regenexx Is Very Different: Hip Labrum Stem Cell Procedure
Every time we have someone visit our Colorado office or one of our network affiliates, they leave dumbfounded about how different Regenexx is from everything else out there. A physician we recently trained commented that when I compare Regenexx to the bedside centrifuges that other doctors use, I often say that what they have is a 10-speed bike compared to the Ferrari we use. His comment, after using a bedside system for years, was that what we use is a spaceship compared to that 10-speed bike. So the above video series will give you some sense of those differences in a hip labrum stem cell procedure.
What Is the Hip Labrum and Why Is Surgery Usually Not a Good First Choice?
Alila Medical Media/Shutterstock
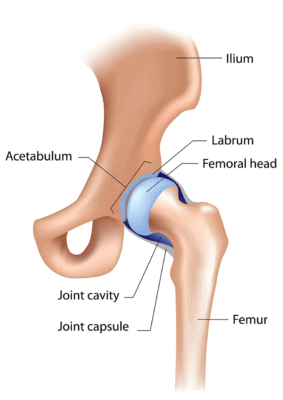
The labrum is the lip around the socket that the ball of the femur fits into to form the hip joint. It helps stabilize the joint, and it can be traumatically torn, or more commonly, it develops tears over time due to aging. Surgeons have been aggressively operating on this structure for the last decade or so. However, there are some problems and side effects with hip labrum surgery:
- It can stretch out the main stabilizing ligament of the hip, called the ligamentum teres.
- Removing one type of hip-bone spur to reduce impingement may be making arthritis worse.
- Many patients without hip pain or problems have a torn hip labrum or impingement—meaning that your MRI showing these things may not explain why your hip hurts.
The Regenexx Hip Labrum Stem Cell Procedure
If you have hip pain that’s due to a labrum tear and you want to try stem cell treatment, here are the types of clinics you’ll encounter:
- The magic-IV-stem-cell clinic. This is usually a fat-based stem cell clinic that will hang an intravenous (IV) drip of stem cells and tell you that these cells will find their way to your hip labrum. The problem here is that 97% of these IV stem cells will end up in your lungs, and since the hallmark of nonhealing labral tissue is that it has a poor blood supply, it’s very unlikely that many, if any, of the remaining 3% of cells will end up in your hip labrum.
- The little-bedside-centrifuge-that-could clinic. This clinic’s physician uses a one-size-fits-all bedside centrifuge to process bone marrow cells. The 10-speed bike discussed above—enough said.
- The blind-injection clinic. This doctor doesn’t use any imaging guidance. Instead, the doctor just sticks the needle somewhere in the vicinity of the hip labrum and calls it good. The likelihood that he or she could get any stem cells into your labrum? Slim and none, and Slim’s on vacation in Texas!
The Video Shows What Regenexx Is All About
The Hip Labrum procedure can help prevent Hip Arthritis which can escalate from mild to severe within a year!
Check out the video above. Note that we’re using two different imaging technologies in this hip labrum stem cell procedure. One is ultrasound, which you have to be an expert in to accurately inject the hip labrum. However, we’re confirming those findings on fluoroscopy with contrast to make sure that the stem cells get to the exact right spot. We’re also using multiple different types of platelet and stem cell injections based on the tissue we’re injecting—the labrum or the hip joint itself.
The upshot? What we do at Regenexx is advanced interventional orthopedics. Your orthopedic surgeon can’t do this using a tiny 25-gauge or 22-gauge needle under guidance; he or she has to rip apart tissue with a scope to get the cells where they need to go. If you want to see what that can do, check out these patients who were left with gaping holes in the tissue where the hip scope was placed. The guy down the street who does some simple ultrasound injections also can’t do this, as this is an advanced skill. Again, as the doctor we trained told us, the difference between the 10-speed bike and the spaceship!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.