How Important is it to Take a Bone Marrow Aspirate with Guidance?
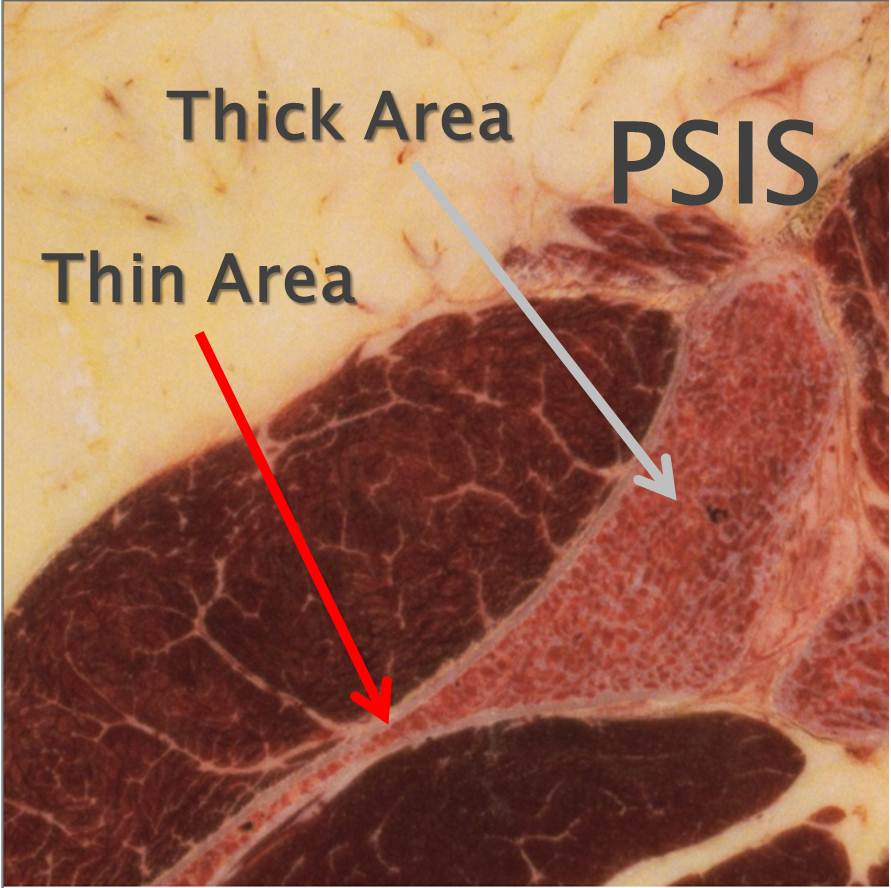
We see more and more patients calling us these days who finally have a few local options for bone marrow stem cell therapy for their orthopedic problems. As the original clinic in the U.S. doing this work, we applaud this expansion of options for patients. However, we also continue to hear from patients that physicians are performing these procedures without any type of imaging guidance. Imaging guidance means that the doctor can see where the needle is going. This is doubly important in the procedure used to harvest the stem cells: a bone marrow aspiration. While many physicians who are just starting to use bone marrow stem cells to treat things like knee, shoulder, hip, ankle, and hand/foot problems may believe they can take an accurate bone marrow aspirate without knowing where the needle is located, a simple anatomy review will show why this isn’t the case. Above you can see a slice through the PSIS area of the back of the pelvis (near the dimples of Venus). This is the most common bone marrow aspiration site to obtain stem cells. Note that the red arrow points to a section of the bone that’s paper thin and that the green arrow points to an area where it’s very thick. These areas are very close together, such that a needle that happens to get into the thin area will get no bone marrow (which is located inside the bone), but simply go through and through the bone, leading to a slow draw of blood that contains few of the stem cells sought. However, a needle that is guided to the correct thick area can easily tap into the bone marrow space and collect stem cells. How did we learn this? 5 years ago as we started to culture cells, we learned it the hard way. A sample from the thin area produced no measurable cells in culture, while a needle into the thick area produced good cultured stem cells. The upshot? When taking bone marrow, a “blind” procedure (without fluoroscopic or ultrasound guidance) is likely to sometimes collect no stem cells. In addition, since the bedside centrifuges used by many physicians have no way to measure what’s obtained (unlike a full level 3 lab), the doctor never knows he’s just taken a bad sample that won’t help the patient, as a bad sample looks just like a good sample!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.