Stem Cell Cartilage Regeneration: What Everyone With Joint Pain Should Know
I love talking to patients in the clinic, as it gives me a never ending stream of ideas for stem cell related blog posts. Social media also provides a way to understand what patients are thinking and we recently received this question about stem cell cartilage regeneration, which I’ll attempt to answer below:
“I recently had an appointment with a Dr X last week, regarding my knee and cartilage degeneration in the lateral meniscus. I asked about stem cell regeneration and was met by if it could be done he would be doing it. He said it is very difficult to sustain the cells in that area. That it still was not accepted as working. He advised that in medical journals and conferences it is no further on and i basically got from him that is a waste of money. Is there concrete evidence it works? Are there MRI’S out there showing severe loss of meniscus and one showing post treatment with a huge increase that i can see???”
Can Stem Cells Regenerate Cartilage?
Mesenchymal stem cells (MSCs) can naturally transform into many tissues including bone, cartilage, and fibrous tissue. There are hundreds of studies of animal models where these cells have been shown to help repair cartilage. In fact, as of this morning there are 1,782 such studies listed in the U.S. National Library of Medicine. So from a conceptual standpoint, we have good prima facie evidence that this can work.
When looking at different stem cell sources, the two most commonly used today are bone marrow and fat. Of the two, there’s much better evidence that bone marrow MSCs can help regenerate cartilage than fat MSCs. So if you had to choose a stem cell source for the purpose of regenerating cartilage, bone marrow would be your best choice. This is why Regenexx uses bone marrow derived stem cells for all of our stem cell procedures.
The Myth of Cartilage Loss as a Primary Source of Pain
Cartilage is the shock absorber that lines the end of your bones. One of the hallmarks of arthritis that’s easy to see on x-rays and MRIs is the loss of cartilage. Given the orthopedic community’s obsession with cartilage loss, you would think we had solid evidence showing that loss of cartilage in a knee is directly associated with increased pain and disability. In reality, there is little evidence that’s actually true.
The largest government funded research studies to date do not relate more cartilage loss to pain. In other words, there are lots of people walking around out there with “bone on bone” knees who don’t have much pain and seem to get along just fine. There are also people with normal cartilage on their MRIs who are in tremendous pain.
So if cartilage loss and meniscus tears usually don’t have much to do with why a knee hurts, what does cause this issue? Frankly, we’re just beginning to unravel this medical mystery. Luckily, we do know a few things:
- There is a toxic “witches brew” of chemicals that live inside the joint that cause swelling and continue to break down the structure.
- There are nerves inside and around the joint that along with the nerves in the spinal cord become “sensitized” to pain signals. These same irritated nerves can cause bad chemicals to be dumped into the joint.
- The bone in the joint can accumulate many tiny microscopic fractures and this leads to bone swelling, which can also lead to pain.
What’s really interesting is that of the MRI findings listed above (cartilage loss, meniscus tears and bone swelling), only bone swelling, or what’s called a bone marrow lesion (BML) is linked to knee pain!
So if Cartilage Loss Has Been Over Hyped, What Should I Care About the Most?
You should care about how your knee functions. Is it stable? This means that all of the ligaments that hold it together are doing their job. Does it swell? If it does, this is a sign of the toxic witches brew mentioned above. Does it have BMLs on MRI? This means the bone is failing and may help explain your pain more than cartilage loss or a meniscus tear. The nerves are also an important factor and consideration.
As far as cartilage is concerned, it’s certainly a good thing to have more. But getting really freaked out about not having an ideal amount of cartilage, or having surgery solely due to a tear in the meniscus that’s visible on an MRI is not a good idea.
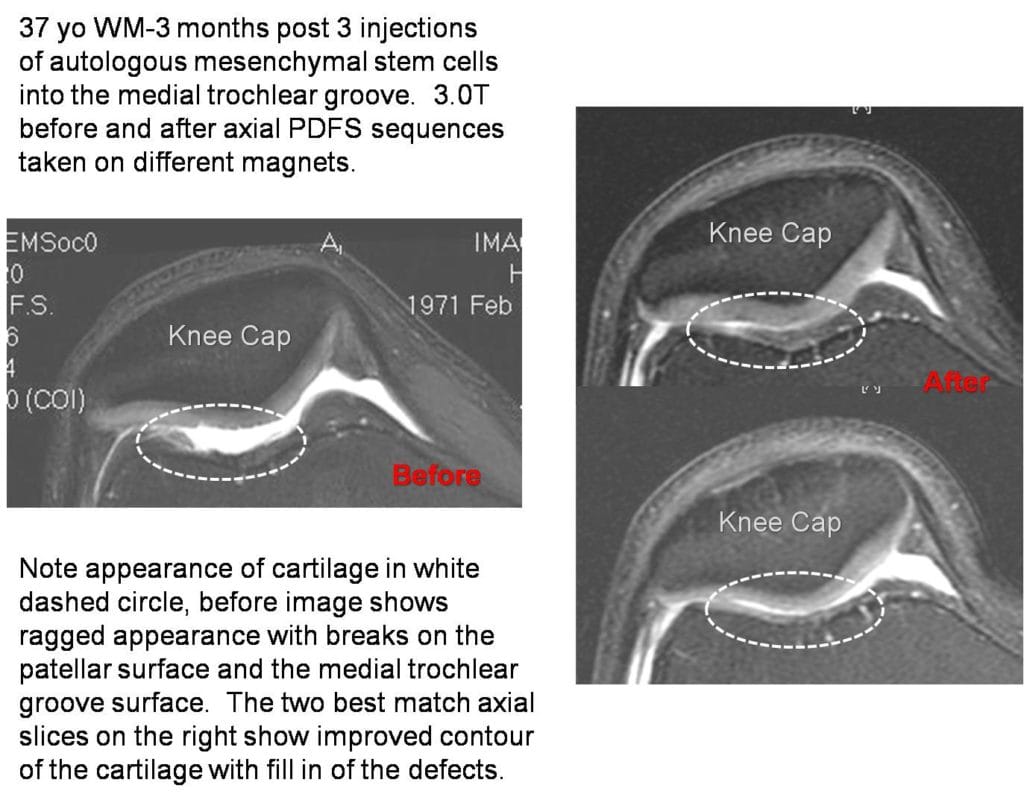
Stem Cell Cartilage Regeneration on MRI
Based on more than a decade of experience in using stem cells to treat knee arthritis, the patients who normally get the best before and after MRI results with regard to cartilage healing are those with smaller holes. For examples of MRIs that show improvement in cartilage following stem cell treatment, see these posts:
- Trochlear groove cartilage defect treated with stem cells
- A cartilage lesion under the knee cap treated with cultured cells
- Improvement in medical compartment cartilage thickness in a patient with only partial thickness loss treated with same day stem cells.
Stem Cells Don’t Regenerate Large Stretches of New Cartilage in Patients with Severe Arthritis, So What Do They Do?
You’ll notice that in all of the cases above, the patient had only a small problem in the cartilage. For example, none of these patients were “bone on bone”. That’s because, in general, we don’t see MRI evidence of cartilage regeneration in patients with severe arthritis.
Having said that, stem cells can do some pretty cool things, all of which are pretty revolutionary. Here’s a list:
- Controlling inflammation by deactivating bad “Pac Man” cells called “macrophages”
- Releasing helpful growth factors that can assist in repair
- Helping dying or damaged cells by recharging their mitochondrial batteries
- Helping other cells produce proteins that can help initiate repair
The upshot? If you have small cartilage problems, a good quality stem cell procedure using precise placement of stem cells into the problem area, performed by an experienced provider, may help repair your cartilage or least make it look better on MRI. If you have a huge amount of cartilage loss, then a stem cell procedure isn’t going to “retread” your knee with loads of new cartilage. Although, in those instances cartilage is somewhat overrated. Stem cell procedures can often provide years of pain relief and improved function in those “bone on bone” patients through a a bevy of mechanisms. So stop freaking out about your lost cartilage and focus on maintaining the healthiest joint possible!
If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.