Stem Cells for Disc Regeneration?
Across the Internet right now, you can find countless websites advertising stem cells for disc regeneration. Is this for real or is it a scam? A recent patient post on our RIP fusion blog can help explain what’s real and what’s likely not.
What Is a Degenerated Disc?
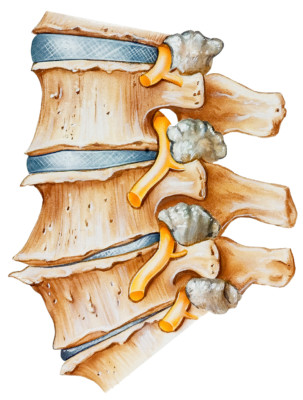
The top two discs are healthy while the bottom two show degeneration. Medical Art Inc/Shutterstock
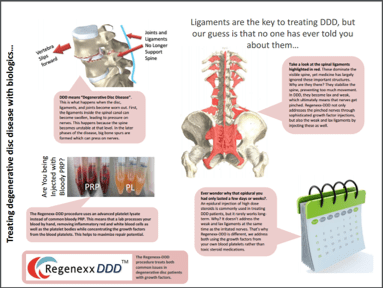
The reason for trying to regenerate a disc is that a disc can degenerate (degenerative disc disease, or DDD). This means that it loses its ability to hold onto water and then slowly collapses. During this process, the whole spinal segment gets sloppy, with too much movement. This is known as degenerative instability.
Why does this happen? There are living cells inside the disc that produce a chemical (called glycosaminoglycan, or GAG) that holds onto water. This ability to retain water is key to the normal function of the disc as a shock absorber that lives between vertebra bones. When the cells inside the disc begin to die off, less GAG is produced and the disc can no longer “plump up,” so it collapses like a leaking water balloon.
Why Are Stem Cells for Disc Regeneration Being Offered?
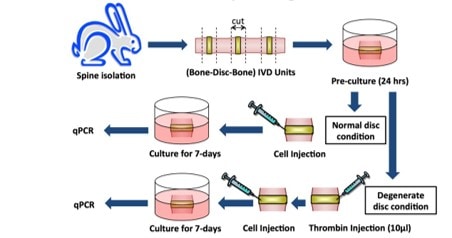
There’s a huge difference between a rabbit and a human disc. First, rabbits walk on all fours, and humans are bipeds that walk upright. As a result, the structure of our discs is entirely different. In addition, experimental studies create a rabbit degenerated disc by sticking what would be the equivalent of a ball-point-pen-sized instrument into the center of the disc and sucking out the cells and GAG gel that lives there. This isn’t how human degenerated discs are made, as they occur over years to decades. For example, few patients have ever walked into my clinic and said, “Aliens abducted me last night and placed an instrument inside my disc to suck out the cells, and now my disc has collapsed…”
Back in 2005, based on what had been published, we were the first physicians to attempt using stem cells for disc regeneration. At first we used a same-day procedure, and when this didn’t work, we switched to culture-expanded stem cells (that had been grown in our lab) to more closely match the successful rabbit model. A funny thing then happened—NOTHING. Meaning we were unable to regenerate a single severely degenerated disc on follow-up MRI. While we were able to refine the technology to help patients with disc bulges and minimal degeneration, regenerating a human disc isn’t happening in multiple published clinical trials since 2005 (see disc stem cell study 1 and disc stem cell research 2).
Learning from a DDD Patient who Had Stem Cell Injections
A patient posted on our RIP low-back fusion blog that he had four severely degenerated low back discs with no disc space left. From 11 years of clinical experience, I have never seen a patient with severe degenerated disc disease respond well to having a same-day stem cell product (or even a culture-expanded one) placed into the disc. It was, therefore, no surprise that this expensive procedure didn’t work. Why?
As discussed above, a severely degenerated disc that has lost all of its height has few living cells inside it. In addition, the outside of the disc (called the annulus) that’s supposed to contain all of those cells is also ripped to shreds. While in theory, injecting stem cells inside the disc should help new cells grow, human degenerated discs are an incredibly hostile environment for cells to survive; hence, most cells placed there likely perish.
What Can be Done Using Regenerative Medicine for Patients with DDD?
First, as above, stem cell injections aren’t the answer. Second, websites offering to inject fibrin glue inside the disc to grow a new one are using a debunked technology that failed in FDA trials (but from the advertising, you would think the opposite). So right now, in 2016, there is no reliable way to regrow a severely degenerated disc. Having said that, we treat these all the time with good success. How?
Finally, just because a severely degenerated disc can’t be regrown like new, doesn’t mean that stem cell treatments for discs are all bad. In fact, if you still have good disc height and a painful tear in the disc, a same day stem cell treatment may help quite a bit. Or if you have a bulging disc, specially cultured stem cells may help get rid of that bulge. It’s just severe disc degeneration that can’t be helped with stem cells at this point. The video below will help explain the different disc types in more detail.
The upshot? At the end of the day, don’t get burned by the idea that someone can regrow a severely degenerated disc—it isn’t going to happen. Instead, focus on what can be accomplished using regenerative medicine in 2016, which is quite a bit when you ignore the disc!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.