Do you Really Have Hip FAI or CAM Impingement?

©Regenexx
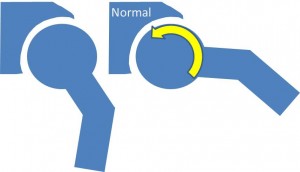
Do you really have hip FAI or CAM impingement requiring surgery? Medicine is like anything else in today’s society, it suffers from trendy diagnoses just like the latest fashion trends. As a result, we’ve seen an explosion in the MRI diagnosis of femoral-acetabular impingement or FAI (aka CAM hip impingement) this past 1-2 years. Just 5 years ago this diagnosis was almost unheard of, but now it seems to have taken over as the trendy hip diagnosis. As with any medical trend, the question needs to be asked, is the explosion in diagnosis warranted or is it being over diagnosed? Our concern is that we’ve seen many patients with a diagnosis of hip FAI based solely on an MRI scan, but real world tests of hip FAI, often fail to confirm the diagnosis. In addition, our analysis of the MRI criteria for hip impingement or FAI caused us some concern. To understand this issue better, it helps to review what’s meant by CAM hip impingement or FAI. The hip is a ball and socket joint, where the outer part of the socket has a rim or lip called the “labrum” (Latin for “lip”). FAI occurs when either a bone spur on the labrum (edge of the socket) or a misshapen femur causes one side or the other to get caught up. As an example, consider the illustration below. A normal ball in the socket hip joint is shown on the left. The right picture shows what happens when the patient moves the leg out to the side, the ball simply rotates in the joint and is free of any obstruction.
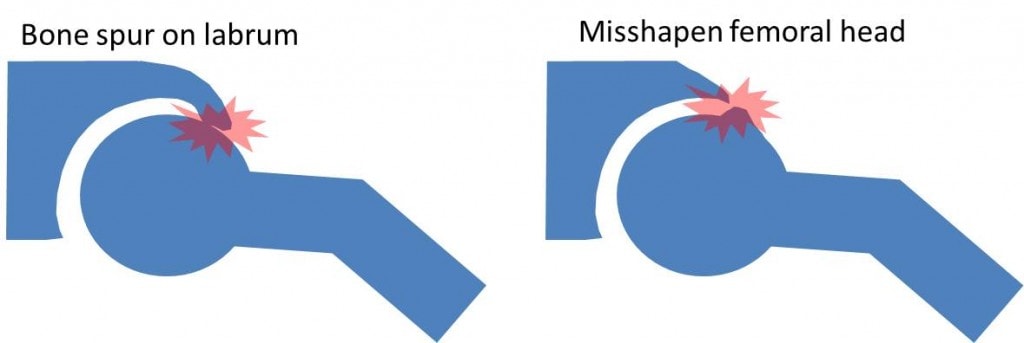
However, every once in awhile, a bone spur on the labrum (socket) or a rough patch on the femur (ball) can cause impingement. In the illustration below, note that the diagram on the left shows a bone spur jutting off the labrum that bangs into the femur as the patient moves the leg outward. On the right, the problem is the opposite, a misshapen femoral head (ball), bumps into outside part of the labrum (socket).
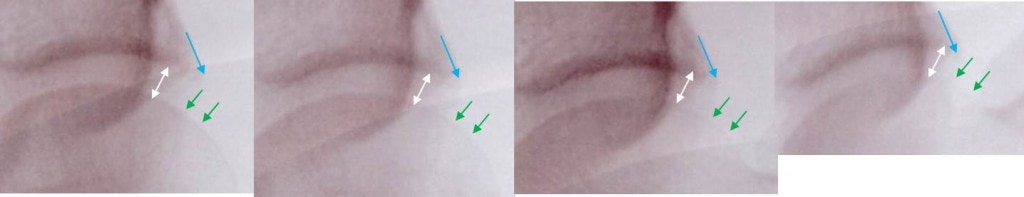
So now that you know what FAI is and isn’t, let’s look at some real patient films. This thirty something patient was seen this week in our Colorado clinic and is a very active cyclist and runner. She was diagnosed with a slight labral tear and hip FAI on MRI. However, her exam in the office looked like most of her pain was actually coming from her SI joint and not her hip (for more information on referred pain, see our medical practice’s book-Orthopedics 2.0). Since hip impingement is something that happens when you move, using a non-moving picture like an MRI to make the diagnosis can be problematic. As a result, moving films to look for impingement are better than static films like MRI. In this case, when we put the hip through it’s paces on real time x-ray imaging, does the hip impinge when moved in certain directions? Her films are up top, with a steady progression of movement of the ball in the socket as the hip is abducted out to the side. I’ve included blow ups of the hip joint below as she moved (simply magnified the pictures up top). The conclusion? There is no evidence of any hip impingement despite the MRI diagnosis of hip FAI. Note the white arrow shows that the hip joint space is maintained while she moves. Also note that the blue arrow (positioned right where the labrum lives), bumps into nothing as she moves her hip out. Also note that the green arrows are where a misshapen femur should bump into the blue arrow, but there’s nothing there to cause impingement in any film. Why the discrepancy? An MRI is just a static image. While we can take certain measurements that might predict who could be at higher risk for impinging, there’s no substitute for moving the hip around and seeing if it actually impinges. An example from common experience would be taking photos of cars standing still and trying to predict, simply based on the picture, which cars have engine problems. In this case, there is no substitute for starting the car to see if it actually runs. In the same way, a static MRI can’t predict with 100% accuracy, which patients are impinging and which aren’t impinging. After all, since the “fix” for hip impingement is an invasive surgery where bone is removed and reshaped, making sure the hip is really impinging should be very important. The upshot? If you have a hip FAI MRI reading which indicates surgery, have a doctor look at your hip under live x-ray to see if it really impinges before a surgeon lops off bone that isn’t impinging anything, and if appropriate tests confirm an impingement, look into hip surgery alternatives which are less invasive and more successful in the long run.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.