Ankle Pain after an Ankle Joint Replacement
The picture above is from a patient seen this morning. She is a middle aged woman who had a mid-foot fusion that caused severe lateral ankle pain and grinding. A surgeon took an x-ray that showed arthritis at the talo-tibial joint and decided to replace that part of her ankle. This caused more severe lateral ankle pain and grinding. What went wrong?

Yok_onepiece/Shutterstock
Regrettably, the association between arthritis on x-ray and pain is pretty weak. Time and time again, research studies show that patients with arthritis or degenerative joints on x-ray are often asymptomatic. We have published on this issue in the low back and the more recent discovery that 60% of knee meniscus tears don’t cause pain, has been blogged on in the past. There is also a recent study showing that pain causes arthritis, and not the other way around. This means that irritated nerves in the joint and presumably in the spine, dump bad chemicals in the joint which ultimately degrades the joint. So with all of this data showing that we shouldn’t rely on x-rays or MRI’s to predict where pain is coming from, why do we see physicians treating the imaging every day? In this patient’s case, an x-ray showing degeneration of her tibio-talar joint lead to that joint being replaced. The pain got worse. Why?
Let’s start with the concept of fusion. A fusion is where the surgeon places hardware (screws and plates) to make a solid structure. Bone is also usually placed in the area to literally grow the two joint surfaces into a solid mass of bone, further freezing motion. The concept began with surgeons treating bony multi-trauma. This was a great advance that allowed surgeons to artificially fix a fracture through surgery and allow the patient much more activity than placing him or her in a cast and in traction. This has been applied to degenerated joints more recently. The theory is that if the joint hurts, fusion will prevent motion in the joint which will ultimately freeze it’s motion and the pain. The problem with fusion is that all joints are connected. Fuse one joint and the motion that should be carried by that joint gets thrown to the next joint in line. This force transfer from the fused joint to the next joint often causes arthritis at the next overloaded joint. The poor next joint in line just wasn’t designed to take that kind of force.
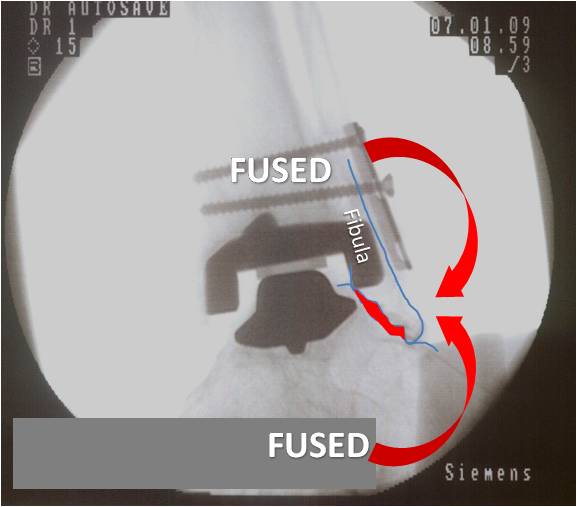
Let’s look at this patients fluoroscope image below. The fibula has been marked and the bottom part of it outlined. The first joints to be fused in the mid-foot (the bottom area marked as “FUSED”) caused those forces to be distributed to the joint between the bottom of the fibula (represented by the red arrow going up). This caused the joint between the end of the fibula and the rest of the foot (marked in red at the end of the fibula) to become overloaded and chronically painful. It likely also caused the other joint up the chain (the tbio-talar or one that was eventually replaced) to become degenerative. However, the catch was that the degenerated tibio-talar joint wasn’t causing pain. So when that joint was replaced (the bell shaped dark colored hardware and the downward facing ‘C” shaped hardware above that) the surgeon also placed the screws to fuse the fibula to the tibia (the area marked as “FUSED” where the screws are located). This then caused more overload of the joint below (the red arrow going down). This made the pain worse, as this was the painful joint to begin with (not the one that was replaced). In the end, both the area below the painful joint and above that joint were fused, causing extra forces from above and below to be relayed into the painful joint. The result, more pain.
Could this have been prevented? YES. The way to prevent this was to perform diagnostic numbing injections under x-ray to see which joint was causing pain. In the end, it would have been determined that the tibio-talar joint wasn’t causing much pain (therefore did not need to be replaced) and the joint between the end of the fibula and the rest of the ankle was causing pain. How do I know this? This morning, injection of this joint at the end of the fibula eliminated her severe pain with walking.
The take home message? Big surgeries in the ankle and elsewhere can have big consequences that are many times irreversible. With the Regenexx procedure, we always take care to first diagnose where the pain is coming from before deploying cells at that location. If needed, this includes diagnostic numbing injections. The same should hold true for any patient considering a joint replacement. Just because the joint looks bad on x-ray or MRI doesn’t mean it necessarily causing pain!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.