Back Pain Won’t Stop? Multifidus Research Update
Most patients don’t realize that if their back pain won’t stop that there’s usually a simple reason that’s invisible to their doctor. In addition, it’s hiding in plain sight on their MRI images, it’s just that nobody with a firm knowledge of the research on chronic low back pain has ever looked. This finding is called multifidus atrophy and it’s a horribly disabling problem.
The multifidus is the most important muscle you doctor has never heard of. It lives deep in the low back and is the major stabilizer of your spine. Anything you do, requires a strong “pre-contraction” of this muscle to prevent chaos in your back bones, discs, joints, and nerves. In a normal back, about 100 milliseconds before you reach to lift something up, this muscle contracts to protect your spine. In fact, when you do anything typical that results in a low back “blowup” it’s usually because this muscle was too weak to do it’s job. Why then has no one ever talked to you about the fact that this muscle is 70-90% atrophied (i.e. abnormally weaker and smaller) on your MRI? This is regrettably more a function of our money fueled medical care system than anything else. Since there are more than 100 research papers on multifidus atrophy and back and leg symptoms, the radiologist should know as should your spine surgeon. But since there’s no way to monetize this knowledge with a surgery or procedure, the problem is ignored by everyone other than physical therapists, who have led the research charge.
The practical problem with getting the muscle stronger is that measuring atrophy has been so expensive. The most reliable way to track whether we’re getting the muscle stronger is an MRI. With managed care raging now due to the ACA, getting one MRI on a patient’s low back is hard enough, but getting serial MRIs (i.e. one every month to see if the atrophy is going away) is almost impossible. As a result, we’ve long sought a way to use ultrasound imaging to measure the atrophy as this would allow us to look at the status of the muscle whenever we wanted. However, the measurements aren’t that accurate as the machine has a hard time telling the difference between healthy muscle fibers and unhealthy fat atrophy at this depth in the body. However, a new type of ultrasound technology may be a game changer.
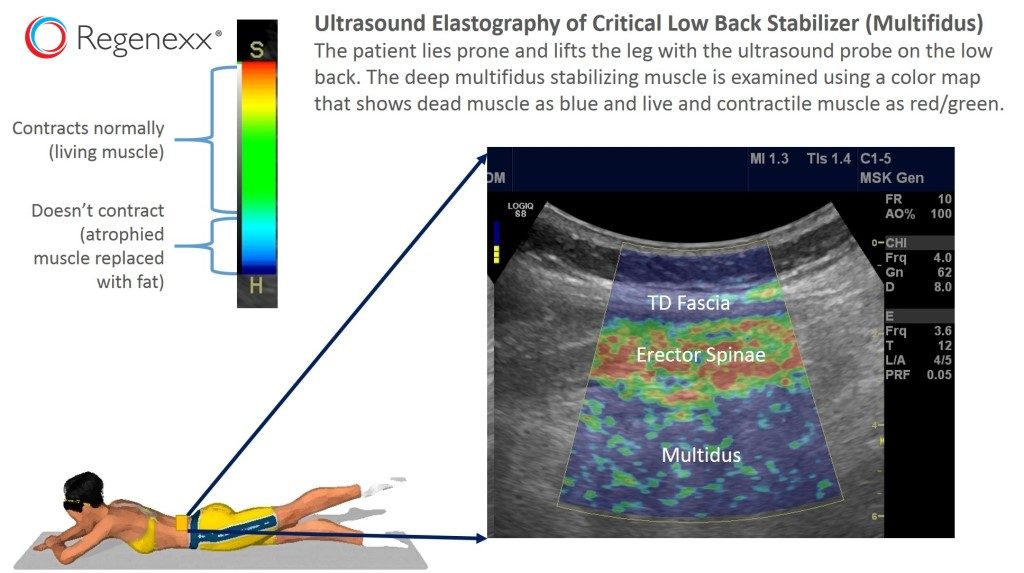
Ultrasound elastography is normally used to help diagnose soft tissue tumors. The doctor presses on the area with the ultrasound probe and the tissue squishes and lengthens horizontally. Special software can color code different regions of the tissue based on how much it lengthens, allowing doctors to easily see a tumor, since it will likely be less squishy. A few weeks back, after buying this special research software for our stem cell rotator cuff tear clinical trial, I began to wonder if it could be used to see the multifidus move. Since the atrophied multifidus muscles of many back pain patients contain only a few muscle fibers that will contract, the software would code them one color (red/green). In addition, the fat surrounding the atrophied muscle isn’t going to change it’s length much when the muscles contract, so it would get coded blue by the software. Could this work?
It’s one thing to have a good idea and quite another to either have the time to execute it or have an assistant smart enough to see it through after a quick discussion. I was fortunate enough to have the later in our 2015-16 fellow, Jason Markle, D.O. He quickly understood the concept and executed it brilliantly. Sure enough, my hunch was right, as the first patients we imaged had color maps of their multifidus muscles that looked exactly like their MRI images! Above you can see the superficial muscle fibers in green/red which are the big main back muscles contracting (errector spinae) while the patient lifts a leg. The deep muscles are the multifidus, which are mostly blue (fat atrophy) with streaks of green (muscle fibers).
The upshot? We are now undertaking a validation study to scientifically prove that the method is really a quick and inexpensive way to accurately measure this critical multifidus atrophy. Once we have that data, we will be able to study many different methods to try and get rid of the atrophy and settle on one technique that outshines the others. Having a method to get rid of the problem should allow many of our Regenexx spine patients with chronic pain to finally have a low back that can protect itself! It will also allow us to easily diagnose this problem before a patient’s back blows up!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.