Lateral Knee Pain
The lateral or outside of the knee can hurt for many reasons. The most commonly cited would be a meniscus tear, a cartilage problem, or a lateral collateral ligament issue. Taking those one by one, the meniscus has recently found to be commonly torn in patients without pain, so we need to take meniscus tears with a big grain of salt now (or at least confirm they acre likely causing pain before just assuming they are causing pain). A cartilage problem would mean injury or degeneration of cartilage on the end of the lateral femur or the tibia. Finally, the lateral collateral ligament is the duct tape on the side of the knee that helps to keep it stable, so an injury there can mean chronic pain and knee instability. Today’s patient case report doesn’t have pain related to any of these three and a good example of how MRI’s can both hurt and help diagnosis. This 60 some year old gentleman had years of lateral knee pain when he entered into one of our research studies. His other knee had a stem cell injection into a frayed and torn menscus and this not only helped to restructure the mensicus, but also got rid of much of the bone brusing that was caused by the bad meniscus. However, the knee that’s the subject of this case report didn’t respond. Our initial focus of stem cell therapy was the medial meniscus, which looked horrible on exam.However, he continued to tell us that most of his pain was lateral (where his MRI looked great). So we looked closer.
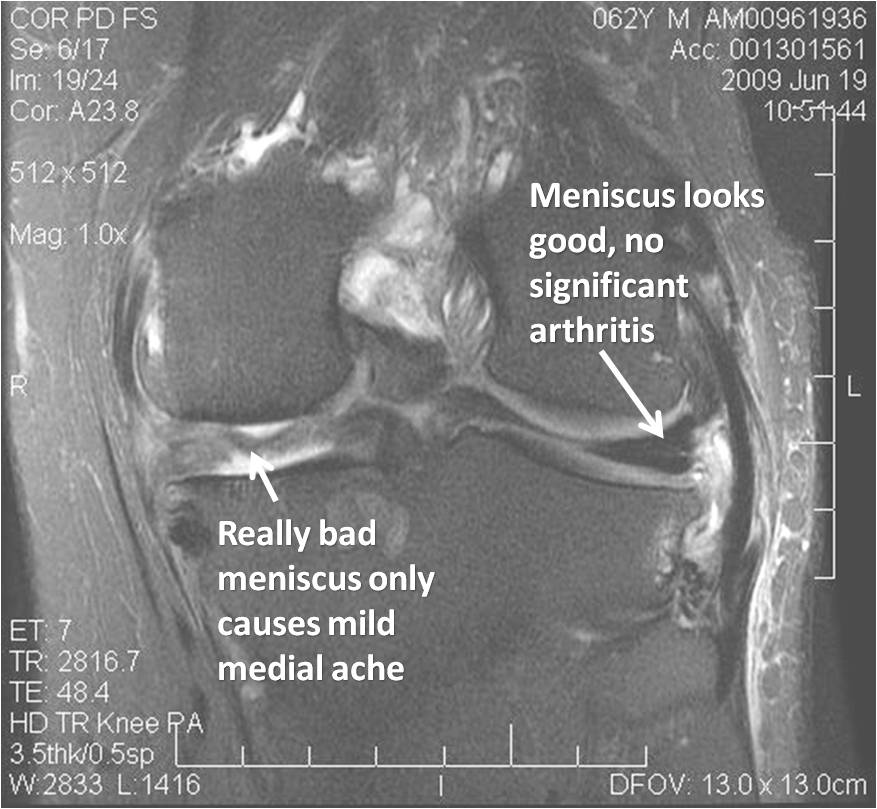
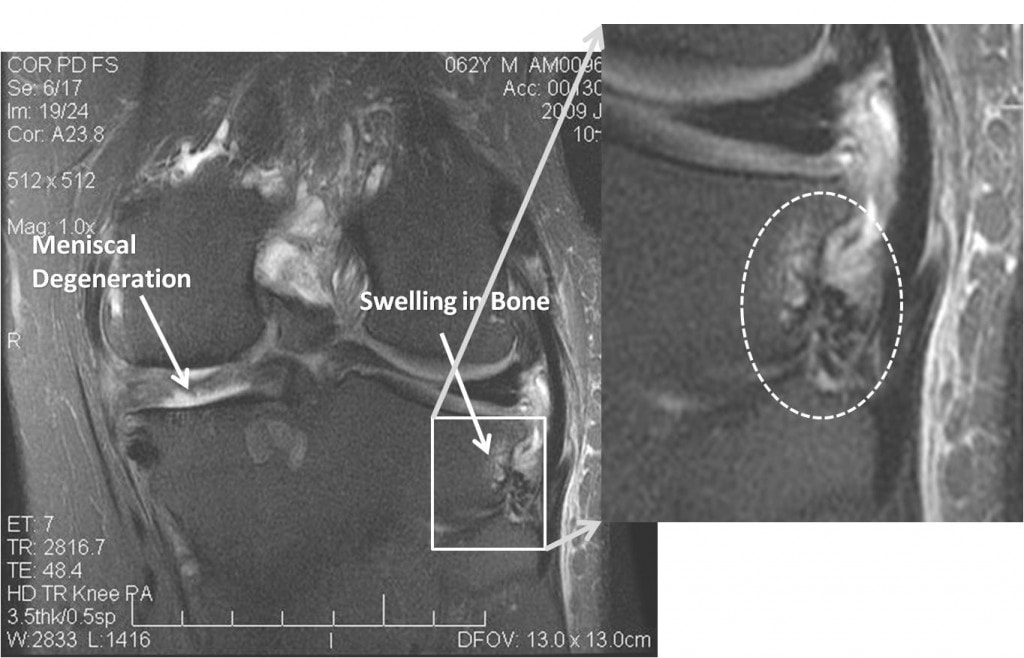
The 3.0 T coronal MRI fat saturation sequence above shows a really bad medial meniscus off on the left, but the patient only has a mild ache on that side. The lateral meniscus on the right side of the image may have some subtle signal changes, but no convincing tears or problems and he is without significant arthritis on that side. He’s also not tender over that lateral joint line. So what’s causing his lateral pain? If we look closer, we see this (picture below):
Notice the bright area in the darker bone in the blown up image (in the dashed white circle). This is swelling in the bone at the lateral tibia, just above where the fibula attaches. Turns out this is exactly where he’s tender, just at the bony origin of the ligaments that hold the fibula to the tibia. On the second round of injections, we focused here, with almost complete resolution of his pain.
I think this case brings up an important issue. As discussed in other posts, meniscus pathology is common in patients without pain, so we need to take all meniscus findings with a grain of salt (great compilation of studies commented on in the NY times at this link). Studies have shown no difference in the amount of meniscus tears seen on MRI in patients with and without knee pain. However, that doesn’t mean MRI is useless, it just needs to be combined with some common sense and the other MRI (my regional investigator or physical exam). We’ve seen this lateral fibular head pain in many patients, often linked into issues with the lateral collateral ligament and iliotibial band.
In summary, operating solely on MRI findings is not a good idea. On the other hand, in our experience these fat saturation sequences can often help sort through multiple issues seen on knee MRI, to find the one that the best candidate for the pain generator. We’ve seen knees with cartilage problems and associated swelling in the bone on fat sat images, while other issues in the same knee have no associated increased signal (and aren’t tender on exam). So in conclusion, always trust exam first, MRI is for correlation only. Or as a old friend told me once, “If you listen to the patient he or she will always tell you what’s wrong, if you listen to the patient long enough, he or she will tell you how to treat it…”
This patient was treated with the Regenexx-C (cultured stem cell injections).

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.