My Brother’s Messed Up Patellar Tendon and Stem Cells
My brother has been a lifelong runner. So when he ruptured his patellar tendon playing tennis and then had it surgically repaired, the big question was whether he could return to running. The answer? Not until some stem cell help. Let me explain.
The Patellar Tendon
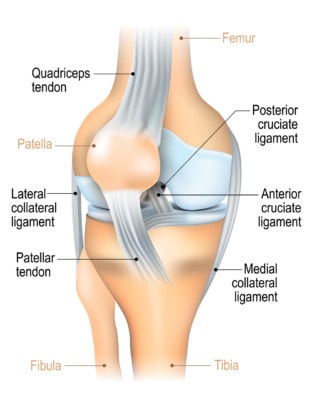
Ligaments of the knee. Designua/Shutterstock
The patellar tendon attaches the bottom of the knee cap to the leg bone (tibia). It’s more commonly degenerative and beat up, but in rare instances, it can completely rupture. When that happens, the knee cap ends up in the lower thigh, and the only option is a surgical repair.
My Brother’s Injury
My brother was a high school and then college cross-country runner for the Naval Academy (he’s the guy in the “Creek” jersey above) and then became an avid jogger once he finished the academy. One day he was playing tennis and then cut suddenly and ruptured his patellar tendon. Given the massive tear and retraction of the patella, there was no other option but surgery. However, his running was never really the same after that. In fact, it was painful to watch him hobble. After several years of hobbling around and pushing through pain, he finally got to the point where he couldn’t run, which is about when I entered the picture.
The problem for my brother was that like most surgical repairs, his was far from perfect and never fully healed in a way that matched his natural tendon. Meaning on MRI and with a more detailed ultrasound exam, the tendon was a disorganized mess. What do I mean?
Tendon 101
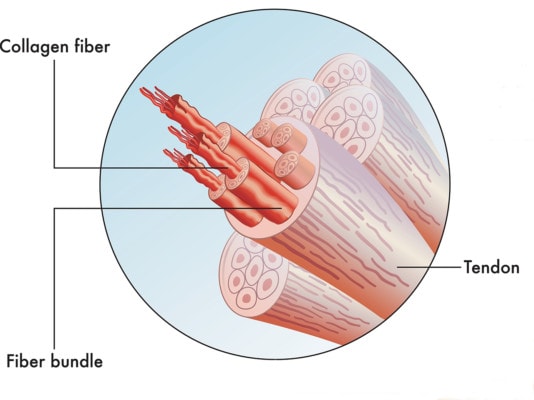
Cross section of a tendon. Rob9000/Shutterstock
In order for tendons to work properly, they need to be organized like strands of a rope. The image to the left shows that collagen fibrils (the threads of the rope) join together to make a fiber bundle (the strand of the rope) and that many bundles make a tendon. As you can see, it’s very well organized. My brother’s tendon had these strands of the rope going every which way, and it was hypertrophied. That last point is key.
Hypertrophy in the world of tendons is likely the most common thing we see that indicates a weak tendon. This means that the body is trying to repair the site by throwing more tissue at the problem, so it makes the tendon bigger. The goal is to get the overall tendon to be stronger so it won’t fail, but the body isn’t able to produce normal dense tendon. Hence, the tendon gets bigger and bigger.
My Brother’s Procedure and Result
My brother had a Regenexx-SD one-day stem cell procedure in April of 2018. I carefully fenestrated this scarred down and disorganized tendon and injected his own bone marrow stem cells. He was in significant pain for a few days, and then things got slowly better as they so often do with tendons. Meaning, full tendon or ligament healing can take a good six to nine months or longer. I knew he was doing better and running more, but I didn’t have a good sense of where he was until he sent me this picture and text yesterday:
“Hi Chris,
Out in HNL… I just ran up diamond head pain free for the first time in years… about a 6 mile trek… thank you for making it possible!”

The upshot? I’m glad I was able to help this messed up patellar tendon and my big brother! There really wasn’t a surgical option here as that would have created more mess. This is one area where only a high-dose injection of his own bone marrow stem cells would do the trick!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.