How Does Prolotherapy Solution Impact PRP and Stem Cells?
We’ve seen a number of providers around the country injecting prolotherapy solution with PRP or stem cells. Is this a good idea? As I’ll show, regrettably, this is a just another example of the stem cell wild west where providers mix and match therapies with little basic science understanding or testing of what’s going on. All of this happens at the patient’s expense.
Understanding Prolotherapy and Osmolarity
Before we explore more in-depth on how prolotherapy solution impacts live stem cells and platelets, let me make sure everyone understands prolotherapy and how it works. Prolotherapy is a basic regenerative-medicine treatment that involves injecting certain extra-concentrated solutions for the purpose of causing a brief inflammatory healing response. When used as a treatment all on its own, it can be effective at, for example, tightening lax ligaments and eliminating pain in the tendons.
To fully grasp prolotherapy and how it impacts stem cells and platelets, it’s first important to understand or refresh your knowledge on some basic physical chemistry. Watching my video above will provide you with some visuals to enhance the information below. First, you need to understand the concept of osmolarity.
Osmolarity is simply the concentration of a solution. Water always flows out of less-concentrated solutions into more-concentrated solutions. The osmolarity of the body, for example, is at 0.9% concentration, the same as saline or salt water. Compare this to the osmolarity of a common prolotherapy solution, which is typically at 10–15%. Because of this high concentration, we would call prolotherapy hyperosmolar (high osmolarity).
Before I dive into prolotherapy and platelets, let me give you an example of how powerful small changes in the concentration (osmolarity) of a solution can be. If I take your red blood cells (RBCs) and put them into distilled water, I will have changed the osmolarity of the solution they normally live in (serum) from 0.9% to 0%. Basically, a tiny change of less than 1%. Despite this small change, your red blood cells will explode in about 10 seconds. Why? Remember, fluid flows from less concentrated to more, so here water flows from the 0% distilled water solution into the RBCs which have a concentration inside of 0.9%.
So what happens to platelets and stem cells in prolotherapy solution? Let’s begin with platelets.
How Prolotherapy Impacts Platelets
Let’s first explore what happens to platelets in saline, which, as mentioned, is the same osmolarity as the body. In saline, the concentration of the solution is about the same as the concentration in the platelets. What this means is that the water doesn’t really flow one direction or the other.
In a prolotherapy solution, the hyperosmolar concentration is a lot higher than the concentration of the fluid inside the platelets. This means the water flows out of the platelets (less concentrated) into the solution (more concentrated), basically dehydrating the platelets and turning them into platelet “raisins.” And while we have no research on how dried-out platelets might perform, injecting prolotherapy with platelet-rich plasma (PRP) is likely delivering broken platelets.
Why would platelet raisins be a problem? Platelets deliver a precisely timed release of growth factors based on what’s going on in their environment. These growth factors then stimulate specific parts of the healing process. Hence, deforming platelets and likely damaging them by dehydrating them likely impacts this precisely timed release of critical factors that assist healing.
How Prolotherapy Impacts Stem Cells
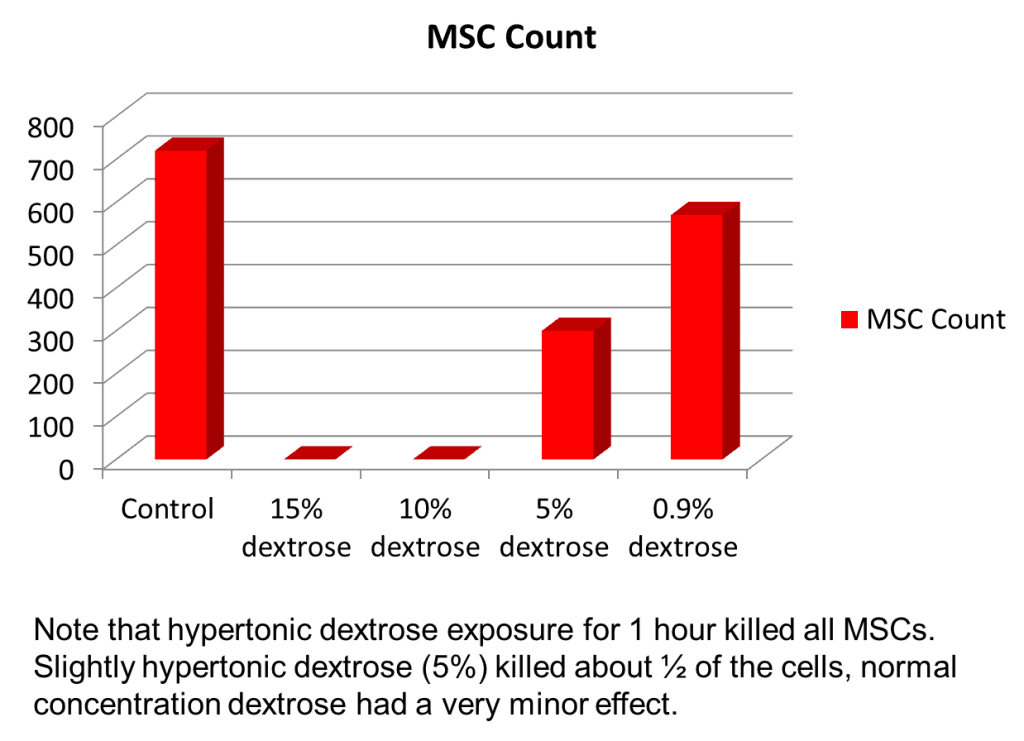
Now let’s take a look at what happens to stem cells injected with prolotherapy solution. We did research on this many years ago. Based on that research, a common 10–15% prolotherapy solution completely killed the stem cells. Even at 5%, a solution that’s commonly used not for prolotherapy but to treat overactive or irritated nerves (i.e., a sweet caudal epidural), caused about half the stem cells to die. So why the toxic effect on the cells? For the same reason discussed above. The prolotherapy solution is hyperosmolar and sucks the water out of the stem cells, causing them to die. Think about it based on your own experience. If someone sucked half the water out of your body in seconds, you wouldn’t last long.
So why use prolotherapy solution for any purpose, and why does it help ligaments and tendons heal? When used alone, it’s a chemical debridement agent. Meaning it purposefully injures, or even kills, the superficial layer of cells in the tissues. This small amount of local cell death causes a brief inflammatory repair cycle. Basically, it gives you another bite at the healing apple if your tissues failed to heal after your initial injury. This is similar to a surgeon purposefully injuring a tendon by making small incisions or a doctor pulling the dead tissue out of a nonhealing skin wound, causing small amounts of tissue damage to prompt healing (debridement).
How Prolotherapy Solution and Cells Can Be Used Safely
Since the osmolar effects of prolotherapy solution take place in seconds, it can be used at a different time than cells. Hence, it can be injected BEFORE the cells are injected. We usually do this days before, so that all effects have run their course before the cells hit the area. It shouldn’t be used right after cells are injected into an area, as that will kill the new cells. However, after the cells have set up shop and helped the repair process, it could be used again (commonly many weeks after the stem cells are injected).
Other Common Injection Protocols that Kill Cells
If you think this little brain slip is a rarity in the wild west of stem cells, think again. In fact, it’s common. For example, orthopedic surgeons and pain-management doctors love an anesthetic called bupivacaine and high-dose steroid anti-inflammatory drugs (e.g., cortisone). Many inject these with PRP or stem cells, not knowing that these substances kill local cartilage and any stem cells being injected. We see many alternative-health practitioners, plastic surgeons, and age-management clinics injecting stem cells IV to treat brain disorders, not knowing that because of the pulmonary first-pass effect, these cells will end up in the lungs and not in the brain. These are just a few examples of the nonsense protocols being used.
Why is this happening? There is no education in residency or fellowship in the cell biology of PRP or stem cell therapy. That means your famous orthopedic surgeon who takes care of [insert sports team name here] doesn’t have a clue about what kills cells, and what he does know about orthobiologics could fill only a small pamphlet, and most of that would likely be inaccurate. The same holds true for countless doctors who took a weekend course on the subject. It’s even worse for alternative-health practitioners, who have much poorer science backgrounds than physicians.
The upshot? When you hear of an injection protocol like “we inject prolotherapy solution with cells,” question everything. Ninety-nine percent of the medical doctors, chiropractors, naturopaths, and acupuncturists offering “stem cell therapy”don’t know what they don’t know. Meaning, many put together homegrown injection protocols that kill the very cells they say will heal your injury. We’ve never done it that way at Regenexx, which is why we have a multimillion-dollar lab facility at our Colorado HQ site. We test these things before we offer them to patients, to make sure that the cells you get are alive and in the best possible health!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.