Shoulder Labrum Surgery No Better Than a Sham Procedure
Yikes, this has been a terrible decade for elective orthopedic surgery. For years studies have come out and pummeled the world’s most common elective surgeries, such as knee “cleanups” and meniscus procedures showing that neither can beat the outcome of a sham or fake surgery. This last year has also been awful as recent research demonstrated that knee replacement wasn’t cost effective in most patients. Now, based on a new study, we can add shoulder labrum surgery to that list of procedures that can’t seem to beat a placebo.
What Is the Shoulder Labrum?
Alila Medical Media/Shutterstock
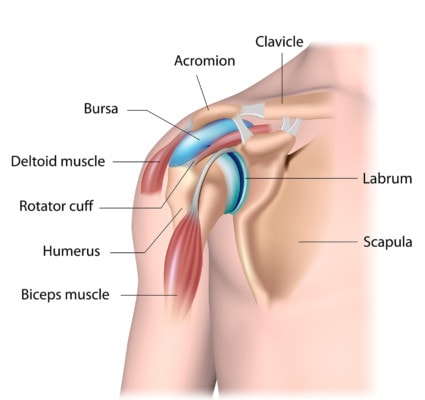
The shoulder labrum is the lip around the socket of the shoulder joint. It’s a fibrous piece similar to a knee meniscus or its cousin in the hip. It can become torn, like the meniscus in the knee. When a patient reports chronic shoulder pain and an MRI finds a tear, then surgery to “fix” the damage is usually undertaken.
Labrum tears, also called labral tears come in many different flavors. The most common naming system breaks them into types I–IV. This new paper focuses on type II, which is where part of the labrum has pulled away from its attachment to the bone portion of the socket. In this case, there’s usually a small gap between the two structures.
Also, the new research focuses on a type of labral tear known as a SLAP lesion. This injury is a problem with the labrum where the biceps tendon attaches to the structure. This issue is at the top front part of the shoulder socket.
Biceps tenodesis is yet another way to deal with a labral tear where the biceps attaches to the labrum (SLAP tear). In this case, instead of trying to repair the labral tear, the surgeon detaches the biceps from the upper lip of the socket and reattaches it to the humerus arm bone. The shoulder labral surgery side effects are even greater in this surgery as it is a bigger procedure than an isolated labral-tear repair because you’re permanently changing the biomechanics of the biceps muscle.
Shoulder Labrum Surgery Side Effects
One of the common shoulder labrum surgery side effects, re-tearing of the labrum, is completely avoidable. Why? The cause of the torn labrum is rarely determined. Hidden shoulder instability is almost always missed by surgeons as rather than extensive exams, surgical decisions are based on MRI. Given that your shoulder has the greatest range of motion than any joint in your body, it requires millisecond tuned timing of a series of tendons and muscles to keep it in the right position in the joint. When one of these has become lax due to a prior long forgotten fall or other injury, the ball of the humerous is not kept where it needs to be and knocks into the labrum continually, as demonstrated in the short video below. One weight lift, or one reach, or one hang done with both arms can spontaneously result in a torn labrum in the shoulder with hidden shoulder instability.
Other shoulder labrum surgery side effects result from changing the biomechanics of the shoulder. As mentioned earlier, the shoulder is an incredibly complex joint that literally requires an incredible level of precise timing. Making surgical structural changes to that system can create permanent issues.
The healing and rehab from shoulder surgery is very long and very intense. A “cushion” shoulder brace is required for months, and the atrophy resulting from this prolonged immobilization creates yet another of the most common shoulder labrum surgery side effects. Add to these surgical risk and trauma and avoiding the surgery all together becomes the clearly better option.
The New Research
The research was double-blinded and sham-controlled, meaning that neither the assessor nor the patient knew in which arm of the trial they were entered. The 118 surgical candidates (with a mean age of 40 years) were diagnosed with an isolated type-II SLAP lesion. The patients were randomly assigned by a study coordinator to either receive labral-repair surgery (40 patients), biceps tenodesis (39 patients), or sham (fake) surgery (39 patients).
The results? There was no difference in outcome in any of the three groups! Meaning the two invasive surgeries to “repair” the labrum at the biceps attachment or to reroute the biceps were no better than the fake surgery where no surgery was performed! Ouch!
Orthopedic Surgery as a Specialty Is Coming Apart at the Seams
So we can now add the most common shoulder labral surgery to the growing list of invasive surgical procedures that have bit the outcomes dust once compared to placebo procedures or physical therapy:
- Meniscus surgery in patients 35 years or older for any indication
- Knee “cleanup” arthroscopy
- Spinal stenosis surgery
- Shoulder rotator cuff repair for partial tears
You can also likely add in knee replacement for most patients based on a recent study and analysis that showed that it wasn’t cost effective.
The upshot? As Queen Elizabeth II once said, it has been an “annus horribilis” for orthopedic surgeons. Why are the most commonly performed orthopedic surgeries no better than placebo or sham surgeries? These procedures didn’t begin with any research showing they worked. They were simply added to a growing list of procedures that were invented because we could accomplish them, not because we should. Does this mean shoulder labral tear surgery will end? Very unlikely. In my experience, it takes about a decade and at least one or two more studies to finally put a stake in the heart of an ineffective surgery.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.