RIP Shoulder Decompression Surgery: Another Common Orthopedic Surgery Bites the Dust
The orthopedic-surgery research this past decade has been like the Queen song “Another One Bites the Dust.” It seems like every month another randomized controlled trial shows that the common orthopedic procedures that patients sign up for every day fare no better than fake or placebo procedures. The most recent entry is shoulder decompression surgery.
What Is Shoulder Decompression Surgery and Why Is It Done?
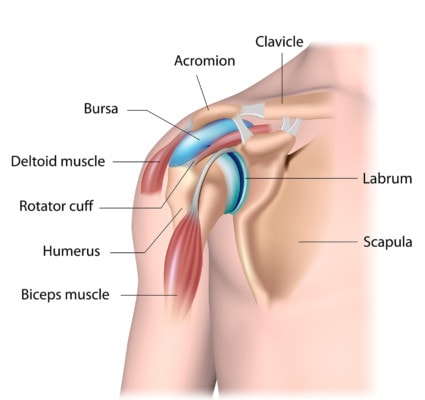
Alila Medical Media/Shutterstock
The idea behind shoulder decompression surgery is that the rotator cuff and its lubricating bursa can become “impinged” by bone spurs and that we need to release the pressure by cutting away ligaments and bone spurs. This extra space will allow the rotator cuff to function better. The idea seems simple, which is likely why the procedure has become so popular.
However, there are problems with the simplicity of this explanation. First, the ligaments that are cut are major stabilizers of the shoulder, so cutting them creates shoulder instability. This means that over time, the shoulder rotator cuff and joints will experience more and not less trauma. In addition, research has shown that rotator cuff tears and their healing after surgery doesn’t correlate well with less pain. In fact, it’s the chemical environment in the shoulder joint that correlates better with pain levels. Hence, the focus here on fixing the shoulder structure with surgery may be a misplaced concept from the start.
Prior Shoulder Decompression Research
I have blogged on a past study that demonstrated that a shoulder decompression surgery wasn’t effective. At the time, many surgeons complained that the images I used for the video on the study were from an outdated and rarely used larger decompression procedure. Despite that, I still see patients who get this bigger procedure. Be that as it may, today’s study is on the more common decompression procedure performed tens of thousands of times a year in the U.S.
The New Shoulder Decompression Research
The new research was massive, involving 32 hospitals, 51 surgeons, and more than 300 patients in the UK. The patients were randomized to either surgical decompression, arthroscopy only (placebo surgery where nothing was done), or no treatment. The results? The surgery groups did slightly better, but those differences weren’t clinically important. In addition, the decompression group did no better than the sham surgery group. In the end, the conclusion was that shoulder decompression surgery is no better than placebo.
Another One Bites the Dust…
“Out of the doorway, the bullets rip, to the sound of the beat, another one bites the dust. Another one bites the dust. And another one gone, and another one gone, another one bites the dust…”
I was keeping track of the percentage of common orthopedic surgeries (costing many billions annually and harming thousands of patients through complications) that have been shown to be no better than placebo or physical therapy. By my back-of-the-napkin calculations, we’re up to about 60% of all elective orthopedic surgeries being useless. How long will it be before US insurers stop covering these invasive, no-better-than-placebo surgeries? I suspect that national healthcare systems, like the NHS, will be the first to eliminate them. In the U.S., so many big players will lose so much money, that I suspect that they’ll be around for a longer time. For example, we have hospitals that wouldn’t be able to make payroll or pay the light bill if they eliminated 60% of elective orthopedic procedures. We have medical-device companies that would declare bankruptcy and lay off armies of surgical-sales reps. Finally, many orthopedic practices would go out of business.
The upshot? Yet another one bites the bust! I suspect that once all of the research now in process is done that 80% of elective orthopedic procedures for pain will be found to be useless. Given that we’re up to about 60% now, we don’t have far to go. We are literally witnessing a historic event: the research base that has supported an entire dominant field of medicine is literally falling apart. Is it time for orthopedic surgery to get a reboot and be reborn as interventional orthopedics?

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.