Cervical Disc Replacement Complications: Metal Ions
We ended the 20th century with the idea that we could cut out parts of a person, like a joint or a disc, and insert metal and achieve great things. Then reality got in the way, in that studies began to show that these metal or plastic or ceramic parts wear down and those particles have to go someplace. This includes into the bloodstream. While this new finding of metal showing up in the blood of patients initially focused on knee and hip replacements, it’s now also showing up in patients who have spinal hardware. The newest data that was just published shows metal ions showing up in the serum of patients who have had spinal-disc-replacement devices inserted.
Rumruay/Shutterstock
The Metal Ion Issue
Metal ions are the atoms of metal that are dissolved in fluid, like water or blood. Joint-replacement devices and implants, though incredibly widely used, have had ongoing issues with raising the concentrations of metal ions in serum (the liquid part of blood). Though the medical-device industry has sought to use new designs and materials to mitigate these problems, the problem seems to have gotten worse rather than better.
Why is having metal or other man-made stuff floating around in your blood a problem? Your body has a very slim margin of error where it likes its fluid to allow its cells to function. For example, if the level of acid (pH) in your blood exceeds a certain amount, you can get quite sick. Or if the levels of certain metals, like cobalt or chromium, exceed a certain minute level, systems as wide reaching as skin, to lungs, to nerves can become an issue. The complications from raising blood levels of metals in the body from the use of various orthopedic implants have been reported, and they are as varied as brain changes, genetic instability, device rejection, and even psuedotumors.
Degenerative Disc Disease
Your spine is an incredibly complex and amazing piece of anatomy that houses and protects the spinal cord and spinal nerve roots. It’s also the body’s central support structure, keeping us upright and connecting the different parts of the skeleton to each other. Although it’s made up of a chain of bones called vertebrae, it’s incredibly flexible due to elastic ligaments, stabilizing muscles, and spinal discs. It has many safety mechanisms and backup systems to ensure proper function, but just like in the rest of us, whether it’s gray hairs, wrinkles, or meniscus tears, the shock absorbers of our spine, called discs, are affected by wear and tear and changes due to the aging process. These changes in a spinal disc can cause it to no longer hold on to water effectively, and as a result it becomes a less effective shock absorber. The disc can also lose height and collapse. But unlike gray hair or meniscus tears due to normal aging, loss of height in a disc does cause problems. The disc becomes unstable and moves back and forth on the disc above and below, which can injure the facet joints and cause arthritis. In response to this excessive motion, your body attempts to stabilize the vertebrae by producing bone spurs, causing a narrowing of the space for the spinal nerves to go through, called stenosis. If enough extra bone is deposited, the bone spur can irritate the spinal nerves, which can lead to neck, back, arm/hand, or leg/foot symptoms.
What Are the Traditional Orthopedic Solutions?
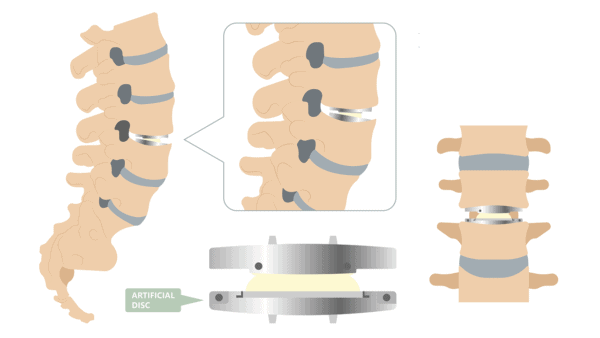
Rather than addressing and repairing any of the failing parts described in the video above that cause instability and resulting bone spurs and so on, in degenerative disc disease, the traditional structural orthopedic paradigm is to fuse the disc solid or to replace it with a metal implant. In a cervical fusion, the disc is removed, a spacer is inserted, and then a rod or plate is used to bolt together the vertebrae above and below. In cervical disc replacement, the disc is removed and then replaced with an artificial disc that is not bolted to the vertebrae above and below. The advantage of the disc replacement is that it still allows some movement while restoring disc height.
The Cervical Disc Replacement Metal Ion Study
The disc-replacement device studied in the new research is made of a titanium alloy and titanium carbon composite and called the PRESTIGE LP Cervical Disc System. The new study sought to compare the blood metal ion concentrations of patients who had these devices implanted with those of other titanium joint replacements and fixation devices. The metal ion concentration was tested preoperatively in 30 patients who had never had any type of metal implant and then tested at regular time points, beginning at one month and lasting throughout seven years post surgery. The results showed that the metal ion concentrations in the participants’ blood were significantly higher at all time points after the cervical disc replacement than they had been before the surgery.
This finding adds a significant new, but not unexpected, entry to the cervical disc replacement complications profile. Load is still passed along to the vertebrae above and below, but, importantly, when something is articulated, meaning two segments are connected by a movable joint, whether it is a hip- or knee-replacement device or an articulated cervical disc replacement system, wear and debris occurs. The difference is, in your natural joints, the wear and tear does not include toxic metal ions.
Considering the Cervical Disc Replacement Complications, Are There Better Solutions?
Rather than removing discs and replacing them with hardware and then dealing with issues like adjacent segment disease and cervical disc replacement complications, like metal ions, nerve issues, and other complications, treating the ligaments and muscles meant to stabilize the vertebrae with precise image-guided injections of your own platelets or stem cells works very well in many cases.
The upshot? The medical-care system continues to promote the idea that you can cut out body parts and insert metal or plastic at will. Why? It’s a huge and big-bucks industry worth in the aggregate hundreds of billions of dollars. However, there is a problem called wear debris, and no matter how you design these implants, wear will occur. In addition, if you continue to advertise these devices to be used in younger and healthier patients who are more active, more wear will happen. Hence, more wear equals more particles, and more particles equals more bad stuff floating around in patients!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.