Dramatic Improvement in Severely Degenerated Cervical Joint Without Surgery
I’ve spent the last 12 years staring at MRIs before and after orthopedic stem cell treatments. I’ve seen some incredible things in many conditions and some MRIs that didn’t change. This past week, as I reviewed the MRI of a patient with a severely degenerated cervical facet joint that we had treated at our licensed facility in Grand Cayman, I gasped. The results were truly remarkable.
Unidentified Instability Leads to Severely Degenerated Cervical Joint: C2-C3 Facet Joint
I’ve discussed before how joints can become unstable (e.g., craniocervical instability, shoulder instability, and hip instability) and havoc can ensue when it goes unnoticed and untreated. This is exactly what happened to the patient whose case study I present in the video above. The patient had been involved in a car accident and experienced a subtle instability at her C2–C3 level in her upper spine. This was not only left untreated but also unidentified. In addition, the answer to her pain, unfortunately, was multiple high-dose corticosteroid injections, and by the time she made her way to me, these injections had likely caused her severely degenerated cervical joint, called DJD (degenerative joint diesase), at the C2–C3 left facet joint, with hypertrophy. This then led to severe foraminal stenosis, a narrowing of the space the spinal nerves run through. This larger facet joint then placed pressure on the covering the spinal cord called the dura.
High-Dose Steroid Injections and/or Surgery Are Bad News
Sure, high-dose steroids, commonly injected into joints to relieve pain, are powerful drugs that may temporarily reduce swelling. Their anti-inflammatory, pain-reducing effects may last for a few weeks or months, and this is why patients feel so good after they get a steroid shot. However, the pain and inflammation returns when the steroid “magic” wears off, often sending patients rushing back for another steroid fix. Why is this a problem? Why are steroids such bad news?
First, pain relief usually diminishes with repeated steroid injections. Research has also linked high-dose steroid injections to many side effects. Their link to cartilage loss is a big one with one recent study showing progressive long-term cartilage loss and pain relief for arthritis no better than with a placebo. Steroids’ effects on bone are also a huge concern as studies have shown associations between steroids and fractures as well as bone loss.
Surgery also would have been bad news. For severe DJD, in orthopedic surgery, cervical fusion would have likely been the last-resort step here. Luckily my patient didn’t get that far. A cervical fusion involves installing hardware, such as plates and screws, to bolt the vertebrae together, rendering them immovable and oftentimes disrupting the normal curves throughout the entire spinal column.
C2–C3 Treatment Without Steroids or Surgery
We initially treated this patient with high-dose platelet rich plasma, which provided good relief of her symptoms; however, because of the severity of her facet joint arthritis, it wouldn’t last. Realizing our culture-expanded mesenchymal stem cell (MSC) treatments were going to be the best solution, in this case, we injected 1 million culture-expanded MSCs and 1 ml platelet lysate at our licensed site in Grand Cayman. This dosage is about a thousand times more MSCs than you could ever inject into the joint within a US-based treatment. We also treated her local ligaments (cervical supraspinous and interspinous ligaments).
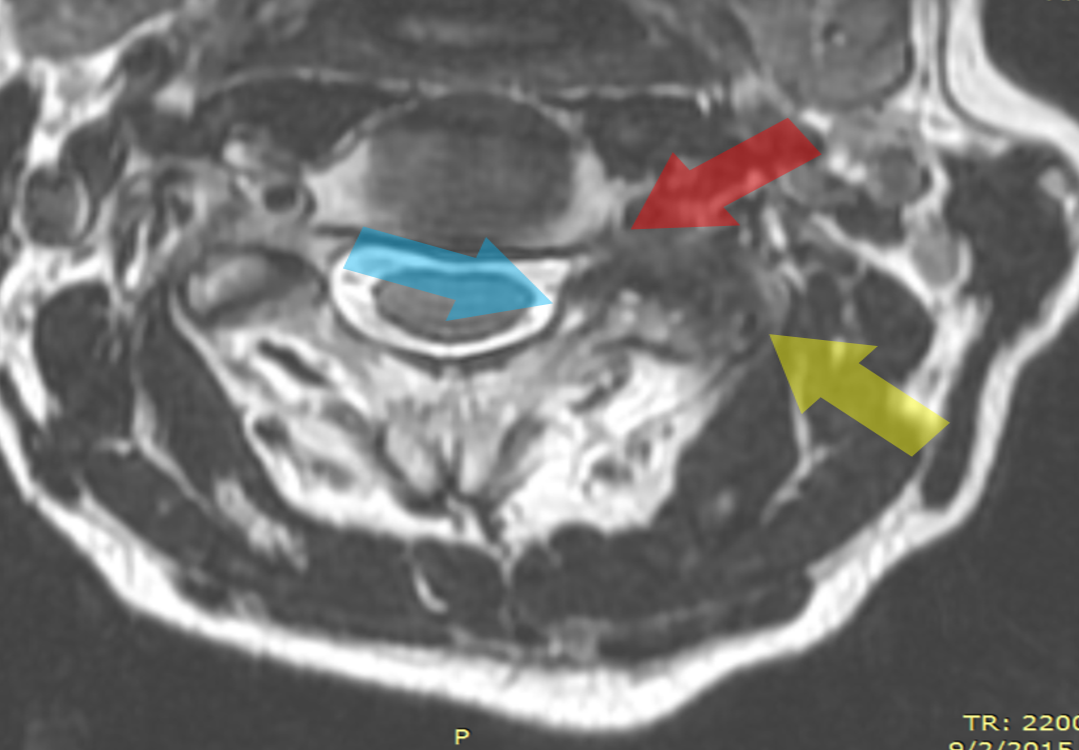
In the video, you will see a dramatic before and after MRIs of the left C2–3 facet joint. First, to look at the before picture, let’s first review the image below. Notice that the facet joint (yellow arrow) is bigger and darker than the opposite side. The darkness means the bone is dying and stressed. The increased size is called hypertrophy. The blue arrow points to the enlarged joint putting pressure on the dura. The red arrow points to the narrowed foramen.
The after image, five months following her treatment (see video), shows her hypertrophy is mostly gone and the bone now appears normal. The left C2–C3 foraminal stenosis and the pressure on the thecal sac, the covering of the spinal cord, has also improved. There was likely still a small bit of fusion in the joint, but considering this was an end-stage joint, this is understandable. Clinically, the patient reports a 60% improvement in her pain.
The upshot? Our advanced stem cell treatments never cease to amaze me. This case, in particular, shows how powerful these procedures can be. Think about it. No surgery, no hardware, and no destruction of the tissues getting all of that done. Just a small needle placed in the right spot to inject the right stuff.
Culture-expanded MSCs are not FDA approved for use in the U.S. but are subject to an existing phase FDA 2 clinical trial. This patient was treated in Grand Cayman, which allows culture-expanded MSCs as the practice of medicine.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.