How Accurate is an MRI for Diagnosing Hip FAI?
MRI is a great tool to help diagnose injury to the soft tissues like cartilage, meniscus, labrum, tendons, etc… However, sometimes it’s too much information and the data it provides doesn’t need to be acted upon. A great example is the recent study showing that 60% of middle aged to elderly patients without active knee pain have meniscus tears.
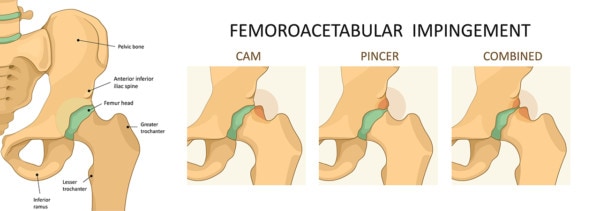
We’ve seen an explosion of late in the diagnosis and treatment of hip labral tears and femoralacetebular impingement (FAI-also known as CAM impingement, pincer impingement, hip impingement, etc…). FAI means that one or both components of the hip (either the ball or the socket) is misshapen and causing the hip joint to impinge (one part of the joint to bang into the other). The types of impingement are listed above (CAM, Pincer, and Mixed-see image below). One website on FAI has a long laundry list of other problems that can cause hip pain that can be confused with FAI. Believe it or not, a lot of other things can cause hip pain other than FAI or hip arthritis. These include: low back problems, SI joint pain, hip bursitis, piriformis syndrome, groin pulls, hernia pain, endometriosis, hamtring pulls, and many other chronic pain syndromes.
Logika600/Shutterstock
As a result, I thought it a good idea to review the published literature on MRI findings. Meaning when the radiologist observes FAI on hip MRI, how certain can the doctor be that this is in fact causing the patients pain versus some other cause. In order for the diagnosis of FAI on MRI to be solid, two main things need to be present. First, the finding has to be found in patients who have the disease (in this case hip arthritis or pain being caused by impingement) and second, the finding (in this case FAI) also has to be absent in patients without the disease (patients without hip pain). This concept is called sensitivity and specificity. A highly sensitive test is one that catches all patients with the disease. A highly specific test is one that excludes everyone who doesn’t have the disease.
So what data exists on specificity for FAI-meaning how many studies have been performed showing that normal people who have no hip pain don’t have FAI? For hip MRI in general, not many studies exist showing how many patients will have MRI findings without pain. I did find one recent study of 21 professional and 18 college hockey players without any symptoms of hip pain. Surprisingly a whopping 77% had abnormalities on hip MRI. How about when we narrow the focus further to only FAI? In this seach, one recently published study is very concerning. This study looked at 200 mostly younger patients without hip pain and showed that FAI was present in 14% of patients (28 patients without any symptoms). A whopping 1 in 4 of the men (24.7%) without any hip problems in this study were qualified as having FAI. Remember, these were younger patients (mean age was under 30 years), so we don’t know if this number would be even higher if we looked at older patients with more wear and tear arthritis. Even more concerning, the alpha angle is often used to diagnose FAI and abnormal is usually considered to be greater than 50-55 degrees. The mean alpha angle in one measurement of these hips was just over 50 degrees (50.1 and 50.2 degrees), showing that the most commonly used measurement to diagnose FAI may not discriminate normal from abnormal patients (at least if 50 degrees or more is used as qualifying someone as having FAI). This contradicts a recent study that only used symptomatic patients who had been surgically treated for impingement or a labral tear, where the “gold standard” number given to make the diagnosis was an angle over 50.5 degrees?
So with only one study of reasonable size using the best quality imaging study (MRI) and normal patients without hip pain finding an awful lot of patients who would could be diagnosed with FAI, the data review this morning on FAI on MRI is not encouraging. If the treatment of FAI were low risk (like physical therapy or a simple injection), would it matter if we wrongly included a lot of patients who had the disease solely based on a picture, but really didn’t have FAI as the cause of their hip pain? Not so much. However, when the the risks of surgically correcting FAI and labral tears are significant, it does matter. 75-80% of patients who undergo FAI surgery for pain get good results, with about 10-15% of patients having increased chronic pain as a result of the surgery. In one study (not designed to ensure 100% reporting of all complications) about 6% of patients had a significant complication which included abnormal bone growth, nerve injury, fracture of the hip, and avascular necrosis of the bone. So the treatment for FAI may be associated with significant complications.
As a result, we would encourage all patients to get an accurate diagnosis before considering FAI or hip labrum repair surgeries. In particular, one helpful and easy test to rule out some of the non-hip causes of hip pain is to numb the hip joint under imaging guidance and determine if this provides significant relief. If it doesn’t, then the patient and the doctor need to look elsewhere for the cause of the hip pain.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.