Hamstring ACL Surgery Complications: Problems in the Hamstring after Surgery
Are there hamstring ACL surgery complications you should know about? I recently blogged on research that showed that using your own tendon resulted in fewer ACL reconstruction surgery failures than using a donor ACL. Many of those ACL tendon grafts are taken from the hamstring tendon of the patient. The particular area that they usually come from is the semimembranosis tendon, a part of the hamstring muscle complex (a.k.a. Hammy). However, what happens when you take away part of a hamstring tendon? Surely that can’t be without long-term consequences. In fact, nobody knows for sure, as few detailed studies have looked at the issue. However, there are no spare parts in the body and a recent study bears that out.
The hamstring is a group of muscles that bend your knee. They start at the bottom of the buttocks where you sit and go down to the back of the leg bone (tibia). They are a common place where tendons are harvested and then refashioned into an artificial ACL ligament when that structure is torn. The surgeon takes a part of one of the hamstring muscle tendons called the semimembranosis. This is then installed at a much steeper angle in the knee than the original ACL, so it’s not quite like a normal ligament. Be that as it may, it’s a mainstay of surgical care. So what happens to the muscle attached to that tendon? Does it suffer?
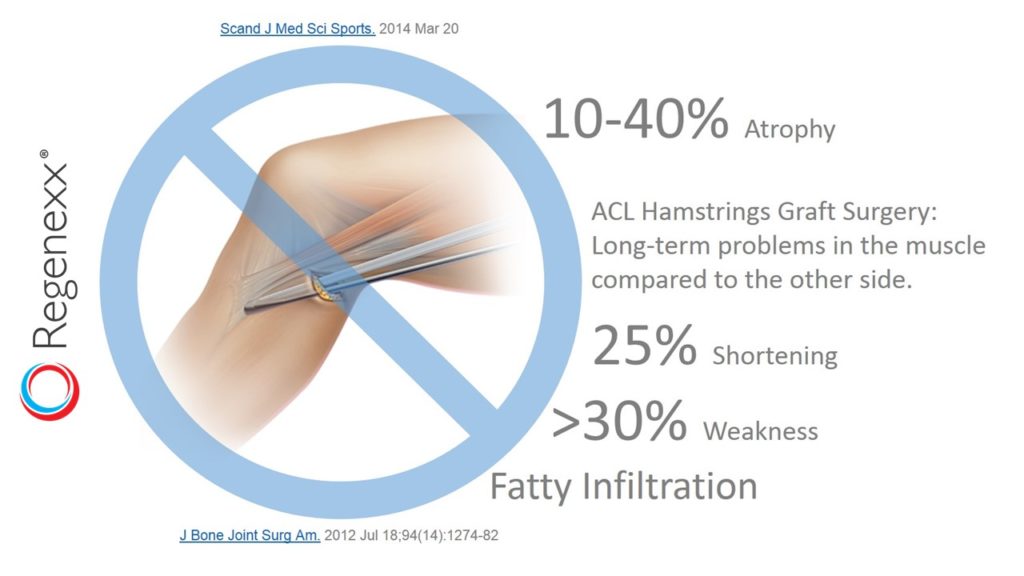
To figure this out, researchers looked at 24 patients and took very detailed post-operative MRI images of the tendon and muscle and strength measurements. What they found wasn’t great for patients who get their ACL’s surgically reconstructed. The good news is that the tendon defect regenerated and filled in for 21 of the 24 patients. The bad news is that the hamstring muscle was 12% smaller and 25% shorter than the non-operated side. In two strength measurements, the hamstring were >30% weaker as well. Another study in 2012 showed similar, but even more substantial issues. In a much longer term follow-up of 9-11 years, the hamstring atrophy was almost 50%! There was also quite a bit of scarring in most patients at the tendon harvest site and the muscle had evidence of dreaded fatty atrophy.
The upshot? This isn’t good for ACL surgery patients, as it shows that removing part of the tendon has consequences. The body is very good at conserving everything and if you make the tendon smaller and/or weaker by cutting out a part of the tendon, the muscle will get smaller, shorter, and weaker. Small changes in how the hamstring muscle functions will have long-term consequences for biomechanics and how the body moves. In addition, this will cause long-term issues in how other parts wear. This is why we treat the majority of our ACL tear patients with a precise injection of their own stem cells into the ACL rather than surgery, as helping the tear heal in place likely results in less long-term biomechanical issues!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.