High Tibial Osteotomy of the Knee Helps Cartilage in MRI Study
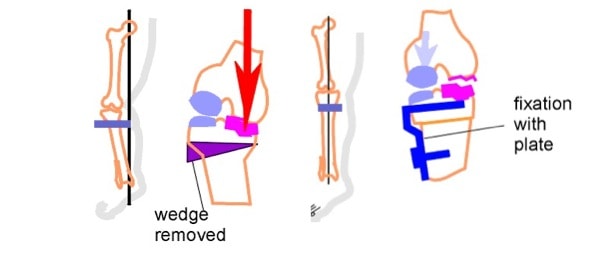
In Latin, valgus means “knock-kneed” and varus, “bow-legged”. High Tibial Osteotomy (HTO) is a surgery performed in patients who have these knee problems. The basic concept is that cartilage is wearing down faster on one side of the knee due to the varus or valgus angle of the knee and the surgery works by removing a wedge of bone from the tibia to straighten out the angle. I’ve always been a little wary of the surgery because it’s a very big and invasive procedure, but the procedure made some biomechanical sense. Now a new study shows that in a small group of 10 patients, the surgery changed the rate of cartilage breakdown on the compressed side for the better. In essence, the MRI numbers for good chamicals in cartilage went from less before the surgery to more after the surgery. The study was very small and didn’t include a group that wasn’t operated. However, to the study’s credit, rather than following patients for only a few months (where the immobilization alone from the surgery would be expected to help the cartilage breakdown) they followed patients for two years and showed that the numbers were still improving after the prolonged immobilization from the surgery. The upshot? While far from conclusive, this study is encouraging for patients who are bow legged or knock-knock kneed who are considering tibial osteotomy knee surgery. Study abstract is below:
Am J Sports Med. 2011 Feb 1. [Epub ahead of print]
Articular Cartilage Changes in Patients With Oseteoarthritis After Osteotomy.
Parker DA, Beatty KT, Giuffre B, Scholes CJ, Coolican MR.
Sydney Orthopaedic Research Institute, Chatswood, New South Wales, Australia.
Abstract
BACKGROUND: High tibial osteotomy (HTO) is a method used to treat medial compartmental osteoarthritis in the knee. The realignment of the knee changes the loading patterns within the joint and may allow for regeneration of articular cartilage. Magnetic resonance imaging methods can be used to assess the quality of the regenerated cartilage.
HYPOTHESIS: Altering mechanical alignment through HTO will have predictable effects on articular cartilage, allowing cartilage preservation and possible regeneration. Quality of regenerated cartilage will be inferior to normal articular cartilage.
STUDY DESIGN: Case series; Level of evidence, 4.
METHODS: Ten patients undergoing medial opening wedge HTO were evaluated using dGEMRIC methods (ie, delayed gadolinium-enhanced magnetic resonance imaging of cartilage) preoperatively and at 6 months, 1 year, and 2 years after HTO. Magnetic resonance images were evaluated by hand segmentation, and T1(Gd) relaxation times reflective of glycosaminoglycan content were determined for these regions of interest using magnetic resonance imaging analysis software.
RESULTS: The lateral compartment displayed higher T1(Gd) values than the medial compartment at baseline. Initially, a decrease in T1(Gd) values on the medial side were observed for all patients at 6 months and remained reduced for all but 2 participants at 1 year and 2 years after HTO. However, on the medial side after 6 months, the rate of change for T1(Gd) values shifted from being negative (-9.6 milliseconds per month) to being positive (1.7 milliseconds per month). A positive change in the T1(Gd) of the medial tibial plateau was responsible for the positive overall change in the medial compartment. There was no significant difference in the rate of change on the lateral side (P = .141), with the average over the 2-year period being a decrease of 2.28 milliseconds per month.
CONCLUSION: Medial opening wedge HTO provides subjective improvements in pain and quality of life, but the potential benefit of allowing articular cartilage preservation and possible regeneration is not well established. Results showed that after a nonweightbearing period, the rate of change in the medial compartment changes from negative to positive, indicating the potential for articular cartilage recovery secondary to an improved mechanical environment.
PMID: 21285442 [PubMed – as supplied by publisher]

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.