Lateral Epicondylitis (Tennis Elbow) – Why There’s Absolutely No Need for Surgery
What is Tennis Elbow (Lateral Epicondylitis)?
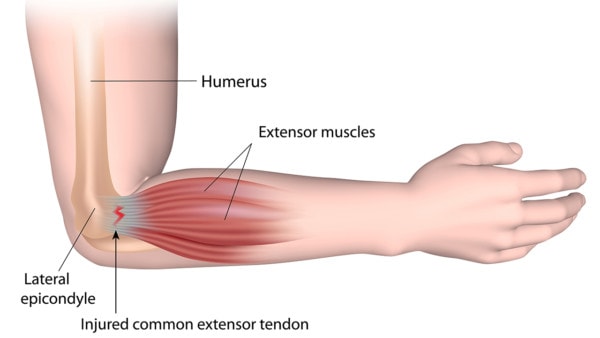
Lateral epicondylitis is the medical term used for tennis elbow which is a painful condition caused by damage or tears in the tendon (common extensor tendon) that attaches the forearm muscle (extensor muscle) to the outside of the elbow bone. Patients suffering from a severe case of tennis elbow find it difficult to do simple things like opening a door or shaking someone’s hand as this movement causes the forearm muscle to extend pulling at the damaged tendon. These certain activities may also cause radiating pain into the upper or lower arm limiting patients to accomplish simple daily activities.
What Causes Tennis Elbow?
Alila Medical Media/Shutterstock
Modern physicians have been fairly agnostic as to what causes the tendon to become painful, as most physicians consider the issue to be due to overuse. We see overuse as being the cause of tennis elbow in patients that perform a repetitive motion for thousands of times a day (like a factory line worker), but more commonly we see patients with some sort of nerve issues in the neck causing the forearm muscles to tug at their tendons. Note that some of these patients never experience any neck pain; therefore the neck is never evaluated and treated.
How Can I Treat Tennis Elbow Without Surgery?
Research has shown that treating patients that suffer from tennis elbow with therapeutic tape helps improve grip strength as well as provide pain relief. [[1],[2]] Note that this is a temporary relief.
Physical therapy is another treatment option given to patients for this condition. Splinting the wrist joint has proven positive outcomes if used while working with physical therapy by providing some pain relief as well as improving grip strength.[3]
When physical therapy and therapeutic tape fails, the next treatment is usually a steroid shot. For many years, doctors have injected high-dose steroids as a short-term fix because this quickly brings down swelling making the area feel better. However, study after study continue to show that cortisone, when used at the high dose that physicians often inject, cause cell death.[4] While causing a little cell injury is not necessarily a bad thing, steroids work by taking away the local repair response leaving you with an injured area that can’t repair itself which makes the problem worse in the long run.[5] More recently, platelet-rich plasma (PRP) injections have been shown to be more effective than steroids.[6], [16]
Tennis Elbow Surgery
A surgical approach is taken when non-surgical treatments such as rest, physical therapy, braces, therapeutic taping and steroid injections fail to provide any relief. The hope with surgery is to clean out the damaged tissue and repair the tear in the tendon that is causing all the trouble. There are two ways to do this procedure.
An open lateral epicondylitis debridement and repair is a procedure that involves a large cut on the outer part of your elbow deep enough to get to the damaged tendon. The goal with this is to clean out any dead tissue as well as repair any tears in the tendon using sutures. Unfortunately, [7]patients that undergo this procedure are in danger of loosing grip strength.[8] Other complications include a late return to work due to prolonged postoperative recovery time, risk of posterolateral instability of the elbow due to ligament injury during the procedure or a formation of a neuroma (pinched nerve) after the surgical procedure. [9]Patients that have this procedure typically are cleared to return to work 2.5 months after the surgery.
During an arthroscopic lateral epicondylitis release, a small incision is made to introduce a small camera into the elbow to help get a better view of the damaged tendon. Patients that undergo this procedure have reported complications such as nerve palsy. This procedure involves cutting the tendon or scoring it with multiple cuts to helps prevent further injury to the surrounding ligaments as well as any potential instability in the elbow.[10] This procedure is an alternative way to treat tennis elbow, but patients should plan on being off work for 1.5 months to recover.
The study shows no significant differences between the 2 tennis elbow surgery groups, including no difference in recovery times–but I would argue that there is no rationale for either one of these surgeries in 99.99% of the patients. [11] [12]
What Is the Best Treatment for Tennis Elbow?
PRP research has shown it to be so effective for this condition that there is little question that this is the definitive treatment for most patients. [13]
Precise ultrasound-guided injections of the patient’s own super-concentrated healing platelets are used to carefully poke small holes in the damaged tendon to get new tissue to grow into those spots. Aside from only treating the elbow, we evaluate the nerves in the cervical spine looking for any pinched nerves or irritation in these [[14],[15]] injecting these as well with the patient’s own platelets to reduce swelling around these areas.
Original Post Date: January 25, 2016
- George CE Sticking to the facts: A systematic review of the effects of therapeutic tape in lateral epicondylalgia. Phys Ther Sport. 2019 Aug 27;40:117-127. doi: 10.1016/j.ptsp.2019.08.011. PMID:31518778 https://www.ncbi.nlm.nih.gov/pubmed/31518778
- Cho YT, Hsu WY Kinesio taping reduces elbow pain during resisted wrist extension in patients with chronic lateral epicondylitis: a randomized, double-blinded, cross-over study. BMC Musculoskelet Disord. 2018 Jun 19;19(1):193. doi: 10.1186/s12891-018-2118-3. PMID: 29921250 https://www.ncbi.nlm.nih.gov/pubmed/29921250
- Kachanathu SJ1 Comparison of the effects of short-duration wrist joint splinting combined with physical therapy and physical therapy alone on the management of patients with lateral epicondylitis. Eur J Phys Rehabil Med. 2019 Aug;55(4):488-493. Doi: 10.23736/S1973-9087.19.05280-8. Epub 2019 Mar 21. PMID: 30916527 https://www.ncbi.nlm.nih.gov/pubmed/30916527
- Pace CS Soft Tissue Atrophy Related to Corticosteroid Injection: Review of the Literature and Implications for Hand Surgeons. J Hand Surg Am. 2018 Jun;43(6):558-563. doi: 10.1016/j.jhsa.2018.03.004. Epub 2018 Apr 3. PMID: 29622410 https://www.ncbi.nlm.nih.gov/pubmed/29622410
- Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet. 2010 Nov 20;376(9754):1751-67. doi: 10.1016/S0140-6736(10)61160-9.
- Gupta PK PRP versus steroids in a deadlock for efficacy: long-term stability versus short-term intensity-results from a randomised trial. Musculoskelet Surg. 2019 Aug 26. doi: 10.1007/s12306-019-00619-w. PMID: 31448392 https://www.ncbi.nlm.nih.gov/pubmed/31448392
- Wang D, Degen RM, Camp CL, McGraw MH, Altchek DW, Dines JS. Trends in Surgical Practices for Lateral Epicondylitis Among Newly Trained Orthopaedic Surgeons. Orthop J Sports Med. 2017;5(10):2325967117730570. Published 2017 Oct 4. doi:10.1177/2325967117730570
- Donaldson CT Lateral Epicondylitis Debridement and Repair Using Knotless Suture Anchor. Arthrosc Tech. 2019 Jul 17;8(7):e775-e779. doi: 10.1016/j.eats.2019.03.016. eCollection 2019 Jul. PMID: 31485406 https://www.ncbi.nlm.nih.gov/pubmed/31485406
- Amroodi MN, Mahmuudi A, Salariyeh M, Amiri A. Surgical Treatment of Tennis Elbow; Minimal Incision Technique. Arch Bone Jt Surg. 2016;4(4):366–370. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5100454/
- Burke NG, Mullett H. Arthroscopic tennis elbow release. Ann R Coll Surg Engl. 2011;93(6):435–436. doi:10.1308/147870811X589227b https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3369326/
- Kroslak M, Murrell GAC. Surgical Treatment of Lateral Epicondylitis: A Prospective, Randomized, Double-Blinded, Placebo-Controlled Clinical Trial. Am J Sports Med. 2018 Apr;46(5):1106-1113. doi: 10.1177/0363546517753385.
- Kroslak M, Murrell GAC. Surgical Treatment of Lateral Epicondylitis: A Prospective, Randomized, Double-Blinded, Placebo-Controlled Clinical Trial. Am J Sports Med. 2018 Apr;46(5):1106-1113. doi: 10.1177/0363546517753385.
- Mishra AK, Skrepnik NV, Edwards SG, et al. Efficacy of platelet-rich plasma for chronic tennis elbow: a double-blind, prospective, multicenter, randomized controlled trial of 230 patients. Am J Sports Med. 2014;42(2):463-471. doi:10.1177/0363546513494359
- Lee AT, Lee-Robinson AL. The prevalence of medial epicondylitis among patients with c6 and c7 radiculopathy. Sports Health. 2010;2(4):334–336. doi: 10.1177/1941738109357304
- Fernández-de-Las-Peñas C, Ortega-Santiago R, Ambite-Quesada S, Jiménez-Garcí A R, Arroyo-Morales M, Cleland JA. Specific mechanical pain hypersensitivity over peripheral nerve trunks in women with either unilateral epicondylalgia or carpal tunnel syndrome. J Orthop Sports Phys Ther. 2010 Nov;40(11):751-60. doi: 10.2519/jospt.2010.3331.
- Barnett J, Bernacki MN, Kainer JL, Smith HN, Zaharoff AM, Subramanian SK. The effects of regenerative injection therapy compared to corticosteroids for the treatment of lateral Epicondylitis: a systematic review and meta-analysis. Arch Physiother. 2019;9:12. Published 2019 Nov 13. doi:10.1186/s40945-019-0063-6

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.