Leg Feels Disconnected? It May Be Your SI Joint
I always love hearing how patients describe what’s going on in their body. This last week, a patient with SI joint instability described her problem as her “leg feels disconnected.” This is such an accurate description that I thought it was worth exploring in a blog.
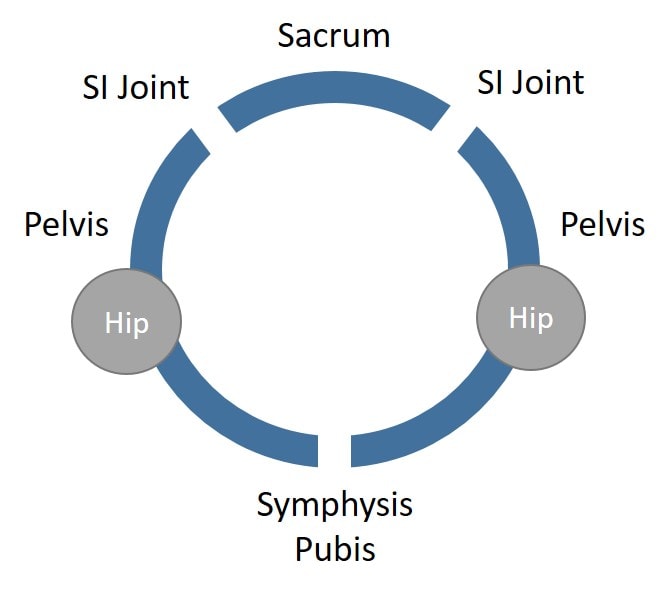
The SI (Sacroiliac) Joint
How the Leg Can Feel Disconnected from the Hip
How Can This Be Fixed?
This patient had been successfully treated 4–5 years ago by using the growth factors derived from her platelets plus a proliferant to help these ligaments tighten. She went from having to wear an SI belt at all times to not having to wear one during normal activities. In fact, the only time she wears her SI belt now is when she’s skiing. She’s now wanting to take the next step and tighten the ligaments further so she can further increase her activities and try to get back to running.
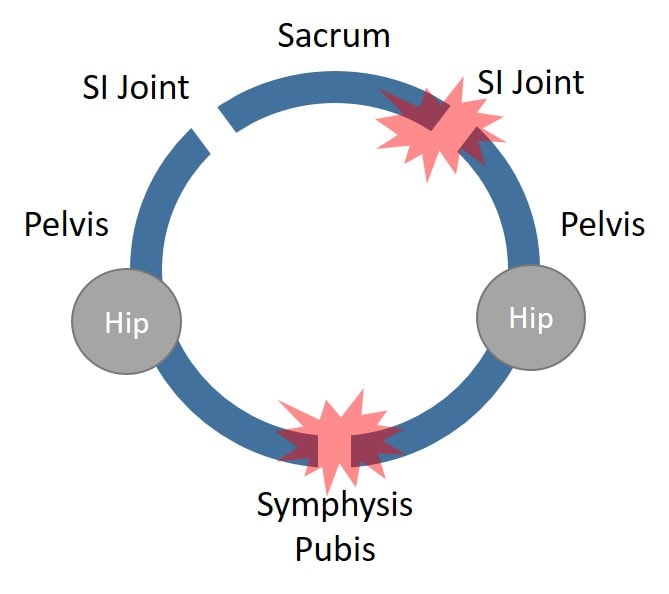
While many of these patients end up with temporary relief from a steroid injection into the SI joint, this does nothing to address the instability causing the problem. Also, most physicians don’t understand that the symphysis pubis joint in the front of the pelvis is as important to treat as the SI joint. Hence, many doctors who offer prolotherapy (ligament injections) don’t treat that area. In fact, this patient was offered that several years ago but demurred. She’s now ready to take that step so we can get more of the pelvic-ring instability under control. So this time, we’ll not only inject the SI joint but use fluoroscopy to target the symphysis pubis as well.
The upshot? I love to hear how patients conceptualize their problem. The famous physician Sir William Osler once said that if you listen to the patient long enough, they’ll tell you exactly what’s wrong with them. In this case, the good doctor was right!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.