You May Have a Pinched Low Back Nerve Despite What Your Doctor Thinks
The first day of medical school, our head honcho got up and was brave enough to say that about half of what they would teach us would probably be proven wrong. Yikes, was he ever right. This also applies to what your doctor thinks he or she knows about back pain. For example, we have traditionally been taught that a pinched nerve in the back causes leg symptoms. However, a study published last year changed that. Turns out, if you have pain in the butt area, whether or not you have any leg symptoms, it’s probably a pinched low back nerve.
The Anatomy of the Back: What Is a Pinched Low Back Nerve?
Rumruay/Shutterstock
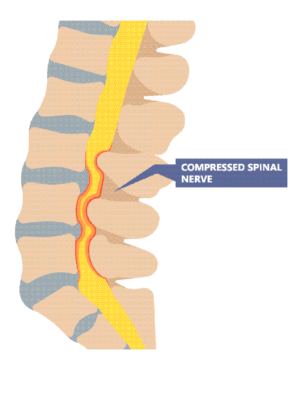
There are a number of conditions that can cause a pinched nerve in the back, but to understand what causes a pinched nerve, let’s first explore the anatomy of the back. The foundation of the spinal column consists of 24 vertebrae, or backbones stacked one on top of the other with a disc in between each level at the front. The disc absorbs shock and provides cushioning for the vertebrae. In the back part of the spine, each vertebra comes together with the next at the facet joint, and these facet joints run the length of the spinal column. The spinal cord is the large bundle of nerves that is housed inside the canal, which is surrounded and protected by the spinal column. These nerves transmit feeling throughout our body.
The low back nerves can become pinched with foraminal stenosis, or a narrowing of the foramen, the tunnels along the spinal column that the nerves travel through. Bulging or herniated discs and arthritis in the joints of the spine can also cause pinched nerves.
The New Study
The purpose of the new study was to explore how pain is distributed in patients who have chronic disorders of the low back. There were over 1,800 subjects with chronic low back pain in the study, and these patients were between 20 and 79 years of age. They were first screened via questionnaire to score their pain and pinpoint the precise location of the pain, which included the low back, butt, and legs. Then they were given a validated questionnaire that can identify whether nerve pain is the main issue. The authors concluded that even if the patient didn’t have leg symptoms, most of the patients with butt area pain likely had nerve issues in the low back. This is opposite what your doctor has been taught, who may still believe that you need to have leg symptom for him or her to take a look at pinched nerves.
Why is this an important study? Many patients with chronic back conditions have pain in their butt. Now that we know that just like symptoms in the leg this can relate back to a pinched low back nerve, doctors can now look at the low back MRI just a bit differently. For example, there have likely been millions of patients through the years with a clear pinched nerve on their low back MRI with butt pain and without leg symptoms who have been told that their MRI doesn’t explain their symptoms!
The upshot? If you have back pain that goes into your butt area, you may well have a pinched nerve in your back. Your doctor may not agree if you don’t have leg symptoms; however, based on this new research, your doctor may need an educational update!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.