What’s Possible with Stem Cell Cartilage Regrowth?
As you may have read some time ago, I got to experience what a cartilage lesion can be like in a young person when my son was 14. On a separate note, yesterday, I looked at the before and after MRIs of a twentysomething we had treated and at the same time got a video of my son, both of which prompted me to write this blog. Like my son, this young man had a hole in his cartilage and was treated using cultured-expanded stem cells in Grand Cayman. So what’s possible with stem cell cartilage repair? Let me show you.
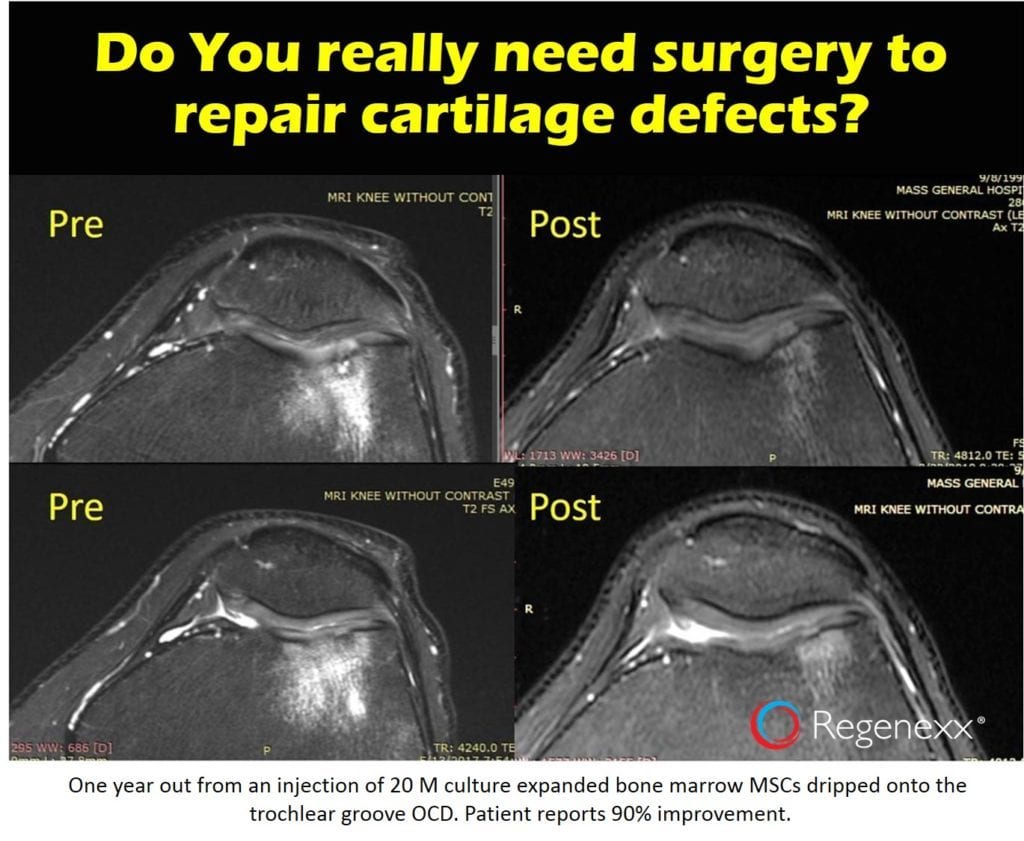
Before and After MRIs
While we have seen small cartilage holes heal with a precise, bone marrow-based stem cell procedure that delivers high doses of cells, what we haven’t seen is cartilage regeneration in severe arthritis. Regrettably, despite having the world’s deepest and broadest experience in this field and making this statement, we’ve recently seen scams run by chiropractors injecting dead amniotic stem cells, calling this a live stem cell injection, and promising elderly people with bone-on-bone arthritis that they will regrow new cartilage. So what’s been historically possible with regard to stem cell tissue repair in orthopedics with the right type of live stem cells and a very precise image-guided injection? See my video below for a smattering of those results:
Surgical Cartilage Repair?
There have been many attempts to “fix” holes in knee cartilage through surgery. None of them are perfect, and all of them are very invasive. One of the oldest is microfracture, where holes are poked in the bone to release healing bone marrow. Another is an OATS procedure, where good cartilage plugs are taken from another part of the knee and grafted into the hole. Then there’s ACI, which involves growing your cartilage cells and sewing that into the hole. Finally, recently MACI has recently come on the scene, which is ACI plus a matrix on which cells can grow.
I’ve seen countless patients through the years who have had each of these surgeries and I’ve never seen one produce a perfect cartilage repair. Microfracture often leaves dead bone behind or large bone spurs in the cartilage. OATS generally produces a roughened cartilage surface. ACI and MACI can generally produce results like the one you see above. Hence, if repair can be initiated without surgery, we can save countless patients from severe complications, such as infection, blood clots, and the need for more surgery.
My Son’s Story
My son was an avid trampoline jumper. He would use this almost as a meditative thing, several times a day or after school. Lost in his thoughts, he would jump for hours. He actually mastered multiple types of flips and was pretty impressive, but at age 14 he began to limp. You know what they say: the cobbler’s son has no shoes. Hence, I mostly ignored his pain for a few months, thinking that in a 14-year-old, this had to go away as he put a hold on the jumping. However, it persisted, and one day I caught him having trouble going up and down the stairs, so it was time for an MRI. When I first looked at the films it was surreal as these looked like some of my patient’s images, surely not my 14-year-old. However, he did have holes in the cartilage with a bone reaction in each lateral compartment. This is otherwise known as an OCD, or osteochondral defect.
Obviously, he needed treatment, and I knew enough not to pull the trigger on surgery as I had seen many of these kids operated on in their teens later in life. By the time they were in their 20s and 30s, they all had significant arthritis. Hence, we first tried high-dose PRP, which, regrettably, did nothing. Then a same-day stem cell procedure (high-dose bone marrow concentrate), which also didn’t put a dent in the problem. Finally, I took him down to Grand Cayman, where he got his culture-expanded stem cells dripped on the lesions. Within a few months, he seemed fine, but as his father, I was always hesitant to get an MRI after the procedure. I think I was way too emotionally close to the outcome. What if, despite his lack of pain, the lesions didn’t heal? That’s one thing in a 50- or 60-year-old, but in a 14-year-old?
Eventually, my son went on to become a big runner. I wasn’t sure how I felt about this because I was always afraid something would happen. In fact, at his first big half-marathon race, through the mountains here, I was terrified that he would develop some problem on the trail and be left out there alone! When he came bouncing across the finish line, I knew that he was finally out of the woods. Hence, when he sent me this video yesterday of him doing box jumps, I smiled:
My Patient from This Week
This patient is a bit older, in his mid-20s, but also had a cartilage lesion. This was due to extreme weight lifting and in the kneecap area, but when I first met him in Grand Cayman, he was not walking well. I injected culture-expanded stem cells without surgery and carefully and precisely dripped these on the lesion. His before and after images are above.
The two images on the left are before the procedure and show a hole in the cartilage and a large BML (the large white area in the dark bone). The after images show interval cartilage healing and almost no BML. His symptom reduction matches these images, so this hole in the cartilage is healing without invasive surgery. I’ll hit this again down at our Grand Cayman site in July.
The upshot? Yesterday was a good day. Using the right technology delivered the right way in the right patients, we can get small holes in the knee cartilage to heal. This injection procedure can help patients avoid the need for a more invasive surgery. However, that process is very different from the magic pixie dust approach used in chiro offices where nurses blindly inject dead stem cells from amniotic membrane or fluid, so buyer beware.
The Regenexx-C procedure is not approved by the USFDA and is only offered in countries via license where culture-expanded autologous cells are permitted via local regulations. This procedure is now part of a phase II FDA drug trial in the U.S.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.