Prolotherapy for CCJ Instability: Keeping Patients Safe
©Regenexx
Patients with craniocervical joint (CCJ) instability will often be offered prolotherapy injections. While much of this is performed blind, some physicians will use guidance. However, while guidance is used, many times it’s not used with contrast. Why is this an issue? Let me explain.
What Is Prolotherapy?
Prolotherapy is one of the earliest regenerative-medicine procedures. It involves injecting a substance that causes a brief inflammatory response and kicks off a healing cycle. Traditionally, most of these injections have been performed blind, which means without guidance. However, a handful of prolotherapists have added fluoroscopy, an imaging technology that uses X-ray and is most commonly used in spine injections.
What Is a Contrast Injection?
Fluoroscopy is an expensive proposition for a practice. While ultrasound guidance is cheaper and allows for superior imaging of the superficial tendons, like the rotator cuff, fluoroscopy excels at seeing all of the parts of the deep spine. When a spinal joint (aka facet joint) or the epidural space (the area around the nerves) is being injected, the doctor uses contrast. This is a substance designed to be seen on the X-ray that tells exactly where any medication or regenerative substance will go. It’s a critical step for a few reasons. First, it tells the doctor if he or she is in the joint in the first place. This is because even though it often looks like the needle is in the right spot, being off just a few millimeters can mean that the contrast won’t go into the joint. Second, it keeps patients safe, as in some injections, you don’t want medications to go to the wrong place. More on that issue below.
The Prolotherapy Fluoro Injection Without Contrast
One of the long-term trends I’ve seen with prolotherapists is the use of fluoroscopy without contrast. This means that they place the needle in what looks like the joint on the image, but they never confirm this with a contrast injection. This is like using a lifeboat but leaving the CO2 cartridges to inflate it behind. So they never have any way of knowing if they’re actually injecting into the joint. Why would you do it this way? Lack of formal interventional spine training. It’s much harder to learn to ensure that your contrast goes into the joint than to learn to just place the needle into what appears to be the joint opening.
A Scary Game of “Which One of These Things Is Not like the Other”
I recently evaluated a young man with possible CCJ instability (loose ligaments that hold the head on). His records demonstrated that a prolotherapist in the Northeast had injected his upper cervical joints, but from reading the notes, there was no mention of the use of contrast. I immediately knew that the doctor was performing these injections as described above, by merely placing the needle into what looked like the joint opening but not confirming his placement. Hence, even though these injections hadn’t worked, I couldn’t cross these upper neck joints off the list as possible pain generators causing his headache. So I set out to repeat them using some anesthetic and platelet rich plasma.
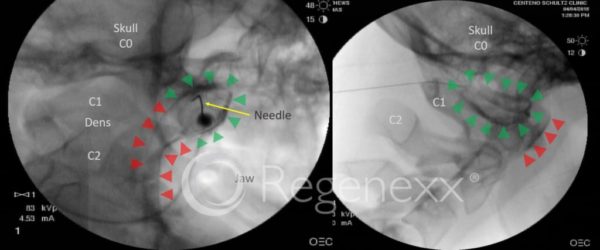
As I tell my fellows, much of medicine is like a Sesame Street game of “Which one of these things is not like the other?” What I mean is that being a doctor is in part about recognizing complex patterns and rendering a diagnosis, but also knowing that the pattern you’re seeing doesn’t fit. In this case, when it came time to inject this patient’s right C0–C1 joint, something didn’t look right on the image. After injecting about 1,000 of these high upper-cervical facet joints, I know they rarely leak. The image on the left above may be hard to interpret, but it clearly shows leakage out of the C0–C1 joint. Let me explain.
Injecting the C0–C1 joint is a dying art. For some reason, it’s mostly not taught anymore to new doctors, and there are only a handful of physicians around the country who have injected 100 or more patients at this site. My partner John Schultz and I have easily injected about a thousand each due to the nature of our practice, so we may have the most experience in the number of C0–C1 injections performed. All that experience allows you to recognize when something isn’t quite right. If you look at the image to the left, the green arrows outline the dark contrast dye in the joint, which in this view is an oval. However, the red arrows mark out what concerned me. This seems to be the contrast dye leaking out of the joint and into an area around the upper cervical spinal cord and nerves. The image on the right is a lateral or side view, and it shows the same thing. The green arrows show the contrast in the joint, and the red arrows show where the leakage has now gone, having accumulated in the far front of the spinal column (the patient was face down). I didn’t show the C1–C2 injection, but it demonstrated the same leakage, going so far as to outline the right C2 nerve root.
A High Spinal Is a Bad Day for Everyone
When anesthetic is injected in the upper neck area, it’s possible to get a “high spinal.” This means that some of the nerves that control breathing can get numbed out and the patient loses the ability to breathe. This is a rare complication of an upper neck injection, and it’s one of the reasons contrast is used as if it looks like the medication will come in contact with these nerves, the doctor needs to change the game plan to keep the patient safe. In fact, in all of the many years I have injected the upper neck, I’ve never had a high spinal by injecting the C0–C1 and C1–C2 joints. Even if something like this were to happen, we have the ability in our practice to handle the issue and keep the patient safe while the anesthetic wears off.
In this patient’s injection, I was able to change around anesthetic concentrations and volumes to both achieve my goal of ruling out his upper neck facet joints as painful and avoid a high spinal. However, as I went through that process, I realized that the prolotherapy doctor who had injected these same areas without contrast would never have seen the issue. Had he actually been in the joint (which he likely wasn’t) and injected a prolo solution containing an anesthetic, the patient may have gotten a high spinal and been in danger.
The upshot? We likely have the world’s greatest experience in injecting the upper neck joints. Experience means that you get to play the “which one of these things is not like the other” game at a higher level to keep patients safe. At the same time, if you go to a doctor who wants to inject your spine and doesn’t use contrast to confirm where the medication will go, then find another doctor!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.