New Regenexx Research Paper on Dosing Publishes
Dose is a key issue in medicine, yet for same day stem cell treatments nobody knows the correct dose nor has a way to measure it so that it can be adjusted to help patients. Huh? You read that right-the entire community of physicians who are using stem cells to treat patients is dose agnostic or to use a better phrase-dose oblivious. Our most recent Regenexx research paper that published yesterday begins to answer some of these critical questions.
We’ve been using stem cells to treat orthopedic conditions allot longer than anyone else, having begun that treatment in 2005. In that time, I can tell you that there are three stages in how a physician interacts with this new technology, as I’ve lived those stages and observe many doctors just entering this field stuck in the first two stages. These are:
- This is magic
- This helps allot of people, but is not magic, just another great tool to have
- Who does this help most and why?
If the doctor just took a weekend stem cell course (which is 90% of the physicians using stem cells on patients today), they’re still in the “This is magic” phase. They have little sense based on personal experience what these cells can really do in specific patients and what they can’t. Their only experience comes from the physician who taught the weekend course and who cherry picked their biggest successes to present, so everything looks like rainbows and unicorns. A few doctors out there who have been using stem cells for a few years have graduated to the “This helps allot of people, but is not magic, just another great tool to have” phase. This is when reality sets in that like any medical procedure, this works for many patients, but some, no matter what you’re using or how, don’t respond. However, very few doctors using stem cells in practice today have graduated to the “Who does this help most and why?” phase. This is where the doctor begins looking at data to see how to turn an art into a more exact science. We’ve been looking at this last phase for years, using biostatistical analysis of our registry data. In fact, it was one of those analyses that birthed this most recent paper.
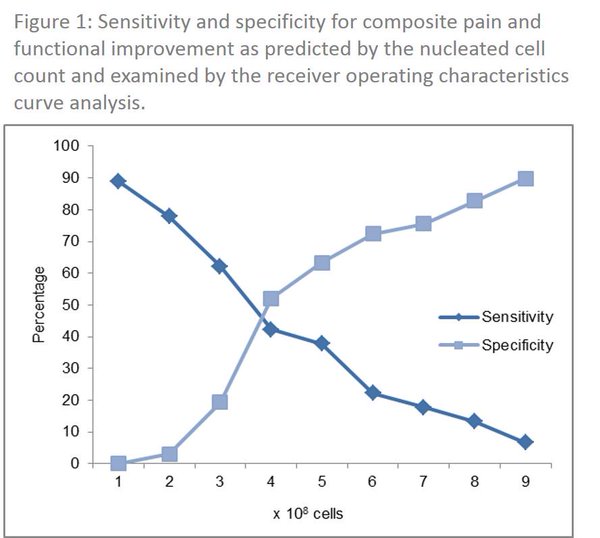
Several years ago we noted that patients in our stem cell treatment registry who had both knees treated just didn’t do as well as those who only had one knee treated. At first we thought that this was because we had identified a group of patients with more severe arthritis (i.e. in both knees versus only one). But the data didn’t support that theory. For example, while patients with 3 or more arthritic joints at the time of their treatment did worse, patients with two joints did not. Hence we began to look at dose. Unlike almost all clinics that do this work, we’ve been counting the total number of cells injected for many years. When we ran the statistics on this information, we saw that patients who got fewer than 400 million cells per knee had less pain relief. We tracked this trend for awhile before we decided to publish on the findings.
What’s really amazing about the new paper is that not only did it find a minimum dose per knee to maximize the chances of success, but the dose counting method is practical to use clinically. This is very unlike the dose metric usually used in medical research-a count called CFUs (Colony Forming Units). This is when a lab places the stem cell sample in culture and the number of colonies that form are counted. While it’s a neat little trick to find a rough estimate of the number of stem cells and is used widely for research, it’s completely useless for finding out the dose of cells at the bedside when that data would come in handy. In fact, it takes a week or so to find out the dose using the CFU method, long after the patient has been treated. Instead of the CFU method, our data shows that a simple total cell count of the sample may act as a proxy for dosing.
The upshot? We’re proud to be well into the third phase of stem cell use-the one where the throw it to the wall art begins to become a science where the doctor can do things to pick the patients who are most likely to respond and adjust his treatment to maximize the chances of success. No rainbows and unicorns here-just using science to stack the deck in our patient’s favor!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.