Surgery to Remove Cartilage in the Knee: Not Effective!
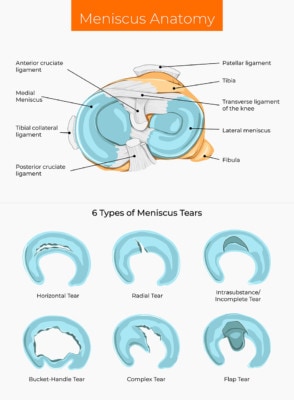
Surgery to remove cartilage in the knee likely happens thousands of time each day. The surgeon pokes in the arthroscope and sees a cartilage flap, a piece of cartilage that is attached at one end and no longer connected to the bone. The doctor then shaves that piece of cartilage off. Why? No particular scientific reason other than it makes the dirty room of the knee look tidier. Now a new study shows that this doesn’t help at all and may hurt the knee.
M_denis/Shutterstock
This Has Been an Awful Decade for Orthopedic Knee Surgery
I saw some pics the other day on Twitter with a bunch of smiling residents and fellows taking an orthopedic knee surgery course. Some were likely learning how to perform surgery to remove cartilage in the knee. I had to chuckle a bit as none of them likely realize that the research train coming down the tracks will derail much of what they’re learning.
The beginning of the end began in 2002, when a Baylor orthopedic surgeon concluded a study that showed that “cleaning up” an arthritic knee (including taking pieces of cartilage and meniscus out) wasn’t effective. The surgeons at the time yelled that this was because of arthritis and that the more focused practice of removing parts of torn meniscus was still a good idea. Then more research was published showing the surgery didn’t work. The surgeons clamored that removing parts of a torn meniscus work well if there is no arthritis. Then another study was published showing that removing the meniscus also didn’t work in patients without arthritis. They exclaimed that the surgery was still needed for patients who had locking in the knee, until of course, a high-level study showed that procedure to be ineffective. Many have still clung to the idea that removing little pieces of cartilage that aren’t fully attached (cartilage flaps) in patients without widespread arthritis is an excellent idea. Until, of course, this new study.
Removing a Cartilage Flap Is a Bad Idea
The new study was a randomized controlled trial. First, it should be noted that the partial meniscectomy surgery on which the study is based has already been shown to be no better than a sham surgery. The patients all had an unstable cartilage injury with a flap and a meniscus tear. They were assigned to either have the cartilage flap surgically removed or not. While there was no difference in outcome at one year between the groups, the patients who didn’t have the cartilage removed actually did much better for the first six months. They had improved function within that time and had more muscle mass at six months.
Why Doesn’t Surgery to Remove Cartilage in the Knee Work?
The parts and pieces in a knee are there for a reason. Even when torn, they do a better job protecting the bone and joint than when they’re gone. So our silly penchant for removing things like meniscus and cartilage is more driven by our desire to make things look pretty than by common or scientific sense. SO NOTE TO ALL ORTHOPEDIC SURGEONS, STOP REMOVING STUFF FROM JOINTS BECAUSE IT LOOKS BAD. IT’S THERE FOR A REASON! LEAVE IT ALONE!
The upshot? Surgery to remove cartilage in the knee doesn’t work. This latest study now means that about 60–70% of all arthroscopic knee surgery is an elaborate sham. That now includes general lavage and debridement, meniscectomy for all indications, and limited debridement of torn cartilage. So when will insurers stop covering this stuff? That, of course, will exit the air from the room for these procedures. My guess is that given the mounting evidence, it won’t be long before the orthopedic knee surgery house of cards comes falling down.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.