Why Middle Aged People Should Ignore Cartilage Loss and Meniscus Tears
The orthopedic community is being turned on it’s head right now. For example, while we have physicians who almost universally agree that cartilage loss in the knee causes pain and/or that a meniscus tear also causes pain, the recent research isn’t cooperating. This blog will be a little more steeped in medical jargon than most, but that’s a necessary evil if we’re going to explore these subjects.
MYTH 1-CARTILAGE LOSS=PAIN
Cartilage is a cushion for a joint that covers both ends of the bone. When you lose cartilage from a joint like the knee, this is one definition of arthritis. Almost every physician and patient I’ve ever met believes that cartilage loss is the cause of knee pain – meaning if you have lost cartilage you must have pain. This is why patients are often hyperfoused on cartilage – is it good, is it bad, how much is there, is there a hole? However, what if the big time research of the last 5 years actually showed that this concept was an urban myth? How would this change everything?
There are two very large, ongoing studies that are tracking patients with knee arthritis with many different modalities such as x-ray, MRI, exams, blood work, questionnaires and biomarkers. These are the Osteoarthritis Initiative (OI) and the Framingham Osteoarthritis Study. Both are sponsored by the NIH and these ongoing studies have felled many orthopedic myths to date, not the least of which is the idea that cartilage loss = pain.
So what do these huge studies say about knee cartilage loss and pain? Does lost cartilage = pain? A recent analysis of the Framingham study data showed that among more than 700 patients who had no evidence of arthritis on x-ray, many middle aged and older patients had MRI findings of arthritis. Here’s what the authors reported in this group:
“The prevalence of (bone) attrition (38% v 30%; P=0.04), bone marrow lesions (59% v 50%; P=0.03), and subchondral cysts (31% v 23%; P=0.04) was higher in participants with painful knees than those without pain (table 2). The prevalences for the other features were within about 4% of one another among painful and painless knees with no significant differences (table 2). Indeed, the prevalence of at least one type of MRI detected pathology (“any abnormality”) was high in both painful (91%) and painless(88%) knees(table 2⇓). Regardless of the definition of pain used, MRI detected abnormalities were highly prevalent in people with (90-97%) and without (86-88%) knee pain. While the prevalence of MRI abnormalities was not significantly different in those with versus those without knee pain for most definitions of pain we tested, the prevalence of “any MRI abnormality” was higher in those with WOMAC pain compared with those without pain (P=0.002). Even so, the prevalence of any MRI abnormality was as high as 86% in those without WOMAC pain.”
So what the heck does all of that mean? Problems in the bone were the only thing associated with pain. All of the rest of the problems seen on MRI that we doctors and almost all patients would think should be associated with knee pain, weren’t. In particular, 72% of patients with cartilage problems had pain, but so did 68% of those without knee pain! These differences weren’t statistically different.
From the other major study, the Osteoarthritis Initiative, despite looking at cartilage loss in almost 500 patients, the amount of lost knee cartilage on x-ray and MRI also wasn’t strongly associated with pain. Let me put the conclusions of these large studies in capital and in bold:
LOST CARTILAGE IN THE KNEE IS NOT ASSOCIATED WITH PAIN OR LOST FUNCTION.
The conclusion of this last study is also important, so it should be in bold as well: Osteoarthritis is a multifactorial process and the need to treat patients based off their symptoms and rely on radiographs as confirmatory modalities, and not diagnostic modalities, when talking about OA and medical intervention.
Translation? If your doctor is looking at an x-ray or MRI and concluding that he knows the cause of your pain without a thorough exam, find a new doctor.
MYTH 2-MENISCUS TEARS IN MIDDLE AGED AND OLDER PATIENTS CAUSE PAIN
M_denis/Shutterstock
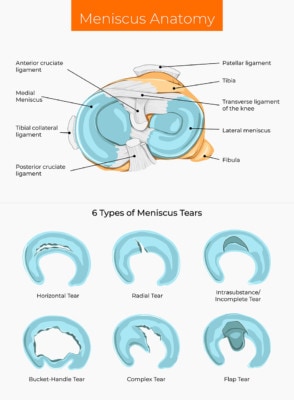
The meniscus is a spacer for the knee that cushions the cartilage surfaces. It’s shaped like a figure 8 and custom fitted for the areas where it snugly fits. It makes some sense that tears in this structure would be considered a big deal. There’s at least some research that a certain type of meniscus tear may be associated with more rapid onset of arthritis. However, we have no idea which came first, the chicken or the egg? Meaning does the special type of meniscus tear cause the arthritis or is it just a feature of the arthritis. Having said that, are meniscus tears seen on MRI important?
Not a second goes by in the US workday that some middle aged patient with new onset knee pain shows up to a doctor’s office with MRI in hand and the conclusion is that the meniscus tear seen on the images is causing knee pain. Also very common is that surgery is performed to cut out that meniscus tear. What if I told you that based on the high level medical research performed to date, this is the one of the biggest medical boondoggle’s of the last century? Let me explain.
The first issue is whether we have any data that a meniscus tear seen on the knee MRI of a middle aged or older person is something that causes knee pain. We’ve known since 2008 based on the Framingham cohort that knee meniscus tears in these patients don’t cause pain (i.e. knees with meniscus tears are very common in patients with and without knee pain). Since then multiple other authors have piled on. In fact, in the study noted above (on a specific group of patients without knee x-ray findings of arthritis but with MRI findings of same) which was published 4 years later, the knees with pain had a meniscus tear 20% of the time and those without had one 25% of the time! In fact, a recent review article by an academic researcher coined a great phrase, that meniscus tears in this patient population are as common as wrinkles and should be treated accordingly.
The second issue obviously is whether operating on these tears does anything to help patients. We have three high level studies that say:
1. Arthroscopic knee surgery to “clean up” a painful knee with arthritis is no better than fake surgery
So in summary, if you’re middle aged and develop knee pain, please don’t fall for the cursory knee exam, quick look at the knee MRI, and conclusion that the meniscus tear seen on the image is the cause of your pain and needs to be cut out!
The upshot? In the knee, orthopedic myths abound. The biggest is that structure=pain. This is earth shaking for orthopedic care, as an entire generation or two of physicians has been educated to look at an MRI or arthroscopy picture with great reverence and that abnormalities that are found are certainly the cause of knee pain. It sacrilegious to many in physicians trained in the 20th century that these sacred cows are falling to the science of the 21st. Knee pain is an incredibly complex thing that involves nerves, bone, and tendons and the only thing on knee MRI that seems to reliably, across most studies, to be associated with pain is a finding that most physicians ignore-bone marrow lesions. In the meantime, as discussed, cartilage loss and meniscus tears, despite the hyper focus of the medical community on them, likely means much less than we once thought.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.