Xiphoidalgia: Should We Cut Out the Xiphoid?
I’ve had a disconcerting brush with what I called “ectomy” pain treatment through the years. My first experience was meeting a patient with testicular pain who had them removed to try and help his agony. This procedure, of course, didn’t work, so that’s why he came to see me. More recently, a patient came in with many symptoms who had xiphoidalgia and who had just had her xiphoid surgically removed. The procedure didn’t go well, so I wanted to explore the concept this morning. Is removing this structure to treat xiphoidalgia a good idea?
If it Hurts Cut It Out
It’s an attractive concept. If a part hurts, we should remove that part. The problem is that it’s usually not that simple. Let me explain via my testicular pain patient.
This guy had seen everyone. Nobody had any answers so a urologist decided that if his testicles hurt, they should be removed. Much to everyone’s surprise, the pain persisted, why?
Pain is a nerve phenomenon. Without the wiring of the body, there is no pain. That’s because pain signals flow from an injured part to the brain as if they were electrical signals along a wire in your house. To understand how complex this can be, think about that wiring in your walls. If the light fixture above your head right now shorts out, it may be the wiring in the fixture. You may also try to replace the bulb and when that doesn’t work, you have a real problem. This is because it could also be the light switch, the wiring in the walls, or a bad circuit breaker. All of these cause the same thing, the light stops working. It’s the same in the body. When a part hurts, it may be that structure causing the pain or it may be the wiring, switches, or circuit breakers of the body.
In the case of my testicular pain patient, what was wrong? It was the “wiring in the walls.” By this, I mean that his real problem was an irritated nerve in his low back (despite the fact that he never thought that he had a bad back). How do I know this? Because we injected his low back nerves with a platelet growth factor epidural and his testicular pain went away for the first time in years.
What is the Xiphoid?
Excellent Dream/Shutterstock
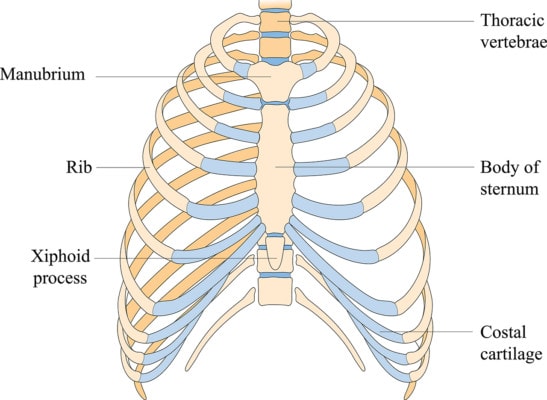
The breast bone is called the sternum. At the very bottom of this structure is the xiphoid, a small piece of bone. This little bone is an anchor point for many important muscles including for the very front of the diaphragm, that muscle that helps us breathe.
Xiphoidalgia and the Concept of Surgery
The patient with severe xiphoid pain came into my office several months ago having just had her xiphoid removed about a month earlier. She had failed conservative care and found a surgeon on the Internet. She was certainly no better one month out and likely significantly worse. That didn’t change over the ensuing month. While I got to know her as a patient, we traded several e-mails, and she sent me a small study performed by a surgeon in Texas that seemed to show fantastic results from surgically removing the xiphoid.
When I dove into this research, I saw something that was concerning. While research can be tough to dissect, given we’ve been publishing patient outcome studies and collecting data on almost 10,000 stem cell treated patients for even longer, this problem jumped off the page. What was it?
The paper (which has yet to be published in a journal) reported on thirty some patients with xiphoidalgia. The methods section of the research study states that the surgeon measured pain before and after removing the xiphoid. The number that looked very out of place was the pre-op pain score. It was listed as a 9.9. Why is that a problem?
A 1-10 pain assessment is called a Numeric Pain Score or NPS. You can’t go to a hospital these days without getting asked about where your pain fits on this scale. 0 is no pain, and a ten is reserved for the most severe pain you could possibly imagine. Most pain patients list their pain as variable in that at times it’s less and at other times it’s more. For example, on that 1-10 scale, the average knee arthritis patient will have knee pain of a low of 2-4 with a high of 5-8. The typical severe pain patient who has something like complex regional pain syndrome (the most painful medical condition known), would generally report their pain as a 6-7 up to a 9/10 and at times a 10. So why was 9.9 a problem?
The pain score of 9.9 in this paper is the average of all patient’s reported pain scores before surgery. If we think about the type of pain scores that would need to be reported to get to a 9.9, it’s pretty staggering. Let’s try some out. Let’s say we had just 10 patients who reported pre-op pain scores: 10, 10, 10, 9, 10, 7, 10, 10, 10, 10. First, this would be a very unusual group of pain patients as I can count on my hands and feet the number of pain patients who have ever reported a 10. Second, the average is 9.4! So if we have 30+ patients, then all of them except 3 patients must report a 10 to get to an average of 9.9. In fact, if even one patient reports a 6 and the rest report a 10, then the average gets pulled down. If this is a mean calculation instead of an average, you get a bit more wiggle room, but not much. So then, what are the implications of a 9.9? This data is almost certainly not patient reported.
I’ve blogged before on what happens when surgeons get to pick the pain scores for their patients rather than the patients reporting this data. The pre-op scores are inflated, and the post-op scores are deflated. I wrote the surgeon who produced this paper and despite several e-mails back and forth, I never got a straight answer as to who reported the NPS data. Even more disturbing is that other case reports of xiphoidalgia don’t show pain scores anywhere near these levels. Again, this supports the idea that the pain score data was someone’s opinion of what the patient was feeling.
The upshot? I haven’t had good experiences with “ectomy” surgeries. The surgeons that perform them almost all universally believe that they work extremely well. The patients who show up at my office, almost all universally don’t get better. While I see a biased population and I’m willing to accept that sometimes these procedures can work, the wonky data contained in this upcoming paper doesn’t make me feel any better about the idea that cutting off the xiphoid is the right solution for most patients.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.